Catatonic depression is one variation of depression that carries a unique power to modify speech, distort movement, and create odd behaviors. Catatonia and catatonic depression are underdiagnosed and could affect as many as 38% of acute psychiatric patients.1 Because this form of depression produces specific symptoms, it requires a specific treatment plan with a focus on medications to reduce symptoms.
What Is Catatonic Depression?
Catatonic depression is different from the most common types of depression because it involves a distinctive group of symptoms affecting movement and behavior. Catatonia is a state in which someone experiences marked disturbances in motor activity. Although generally thought of as reduced activity, it may also manifest as excessive or unusual motor symptoms.
Catatonia may bring about higher morbidity and mortality vs. other forms of depression, but the condition can be treated once it’s diagnosed.1 While catatonic depression is a commonly used phrase, a mental health professional will likely provide the diagnosis of major depressive disorder with catatonia if catatonic symptoms are present throughout the mood episode.
In this situation, the catatonia is only related to the depression, so if the depressive episode resolves, catatonia will stop as well.2
Depression Is Treatable With Therapy
Would you like to feel more happiness and joy? BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you.
Catatonic Depression Symptoms
Catatonia related to depression may occur spontaneously and without warning, but in many cases, the expected depression symptoms will precede the signs and symptoms of catatonic depression. Catatonic symptoms set themselves apart for their severity and their distinctiveness. A person only needs to exhibit three or more of these symptoms to qualify as having catalonia.
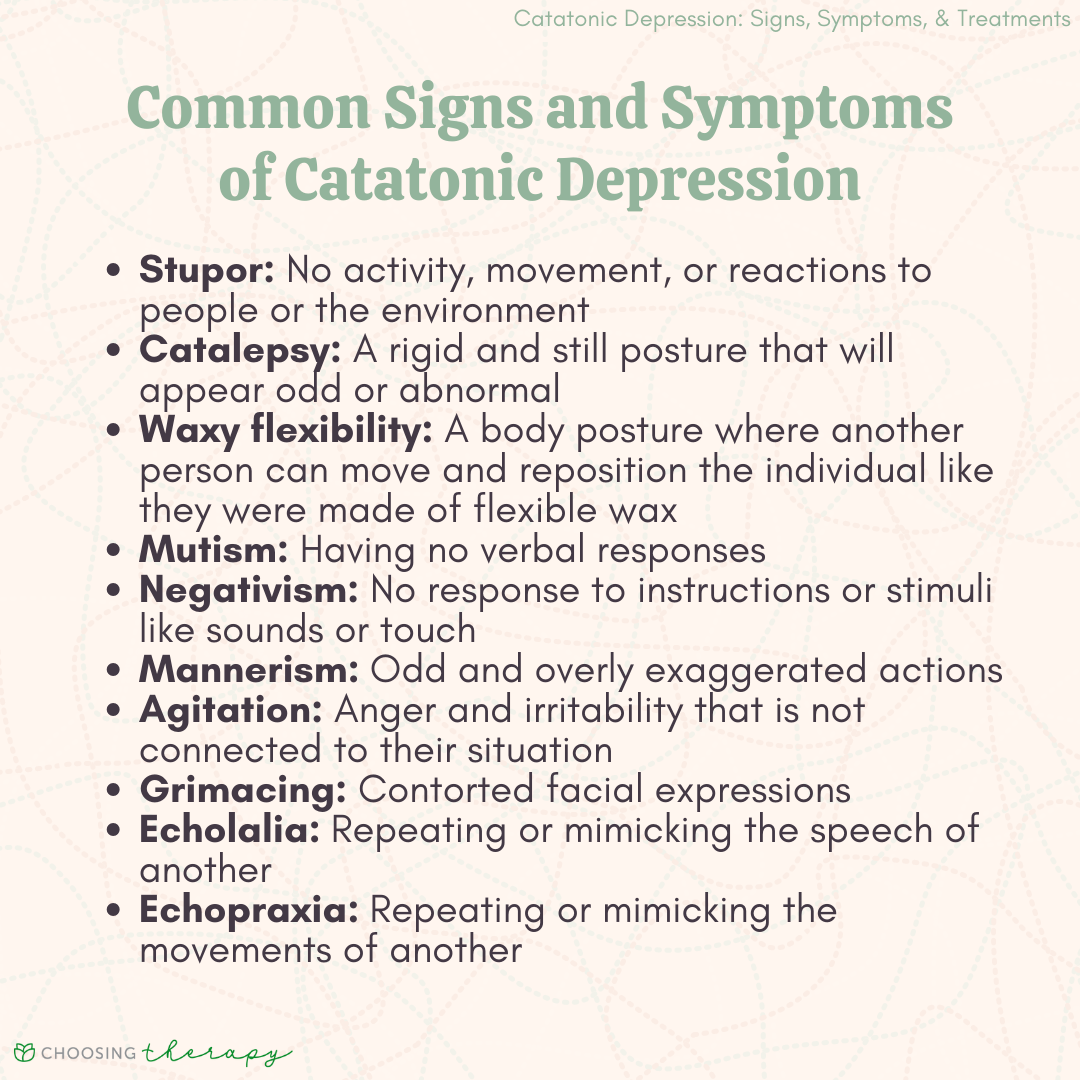
Typical signs and symptoms of catatonia include:2
- Stupor: no activity, movement, or reactions to people or the environment
- Catalepsy: a rigid and still posture that will appear odd or abnormal. A person with catalepsy could be standing with their arm extended or lying with their back arched to the point of only their head and feet touching the floor.
- Waxy flexibility: a body posture where another person can move and reposition the individual like they were made of flexible wax
- Mutism: having no verbal responses
- Negativism: no response to instructions or stimuli like sounds or touch
- Posturing: odd postures like with catalepsy but more active
- Mannerism: odd and overly exaggerated actions
- Stereotypy: repetitive and extremely frequent behaviors
- Agitation: anger and irritability that is not connected to their situation
- Grimacing: contorted facial expressions
- Echolalia: repeating or mimicking the speech of another
- Echopraxia: repeating or mimicking the movements of another
3 Types of Catatonic Depression
With the wide-ranging symptoms and signs of catatonia, one person’s experience with the condition could vary greatly from another’s.
There are three subtypes of catatonic depression:1
1. Stuporous Catatonia
Sometimes called retarded catatonia due to the slowed movements, the person with stuporous catatonia will present with more withdrawn and quiet symptoms. Lack of movement, speech, and self-care are the cornerstones of this type with some people showing automatic obedience where they follow through with any request asked of them.
2. Excited Catatonia
Excited catatonia is marked by excessive movements and disorganized speech patterns. The individual will exhibit rapid and pressured speech while making little sense and jumping quickly from idea to idea.
3. Malignant Catatonia
Malignant catatonia is more frequently linked to physical health concerns or abuse and withdrawal of specific drugs, and is not commonly linked to depression.1
What Causes Catatonic Depression?
The risk factors for catatonic depression include a varied list of physical and mental health symptoms. As many as 20% of people with autism will show the signs and symptoms of catatonia, while up to 50% of catatonia cases are the result of medical conditions.1 Schizophrenia and mood disorders like depression remain serious risk factors for catatonia.
Common causes and triggers of catatonic depression include:1
- Previous experiences with catatonia
- A history of drug-induced movement issues
- Mood disorders that speed up or slow down movements
- Autism spectrum disorder
- Seizures
- Migraine
- Disease or damage to certain parts of the brain, including frontal lobe and brainstem
- Dehydration
- Recent weight loss
- Use of cocaine
- Withdrawal from alcohol and other drugs
- Low levels of iron, sodium, or magnesium in the body
Help For Depression
BetterHelp – Get help from a licensed therapist. BetterHelp offers convenient and affordable online therapy starting at $65 per week. Free Assessment
Talkspace – Online Therapy With Or Without Insurance. Talkspace accepts many insurance plans including Optum, Cigna, and Aetna. Typical co-pay is $30, but often less. Get started
How Is Catatonic Depression Diagnosed?
Catatonic depression is diagnosed by a physician after a series of assessments, including attempts to engage in discussion or interaction. Given that many in a state of catatonic depression can’t verbally communicate, the physician may reach out to the individual’s support system for a history and any trends or patterns they noticed. They’ll do additional tests to ensure there aren’t other physical symptoms happening or other underlying issues.
Why It’s Hard to Diagnose
These very different presentations of catatonia lead to challenges in getting the proper diagnosis. In some cases, a person with stuporous catatonia may appear only to have crippling depression of low motivation and low energy. A person with excited catatonia may appear to have symptoms linked to mania like excessive speech and an increase in energy levels.
To complicate matters, a person could exhibit symptoms from two or three types of catatonia at once to create a mixed presentation that is even more problematic to identify and treat. If a person is feeling symptoms that are extreme or atypical compared to other depressive symptoms, catatonic depression could be the culprit.
Treatment for Catatonic Depression
Because of the unique nature of catatonia, experts use a set of interventions more focused on medication to resolve catatonic symptoms. When catatonia improves, the typical treatment plan involves the combined use of therapy and antidepressant medications.
Before any treatment can move forward, the treatment team must be sure to diagnose the condition accurately. Mislabeling symptoms as being related to mania or catatonic schizophrenia could mislead treatment and create worsening symptoms.
Medication for Catatonic Depression
Medication is the first line treatment for catatonic depression. Common medications used to treat catatonia include benzodiazepines, carbamazepine, zolpidem, muscle relaxants, and tricyclic antidepressants.8 Lorazepam, known by the brand name Ativan, is the preferred medication for children and adults with catatonic depression.5
Although lorazepam is not approved specifically for catatonia, it has been shown to be effective as an off-label use and therefore remains a first-line treatment. Catatonia can be severe and oftentimes require hospitalization. Intravenous medications, specifically lorazepam, are administered in order to minimize symptoms in the most time efficient manner. Once acute symptoms begin to resolve, oral benzodiazepines can be administered.
Therapy for Catatonic Depression
Once the catatonic symptoms are minimized or resolved, depression therapy can play a major role. Other people who have already endured a period of catatonia can work with therapists to better identify warning signs of the condition. From there, they create a prevention plan that lists people to contact and coping skills to use in order to keep it from escalating again.
CBT for depression and interpersonal therapy (IPT) can drastically reduce depressive symptoms in as little as 12 sessions. With this being the case, someone can feel much less depressed in three months or less.6
Electroconvulsive Therapy
In typical cases, a combined approach using psychotherapy and antidepressants is enough to stem the flow of depression, but since catatonic depression is atypical, it may require the use of electroconvulsive therapy (ECT).1 Though ECT may have a negative reputation because of harsh methods used in the past, the treatment, which involves passing an electric current through the person’s brain, is much safer today.
Of the 20% of adults who do not respond to the lorazepam treatment, about 80% from that group will respond to ECT or a combination of ECT and lorazepam.1, 5 ECT, under the care of medical professionals at an inpatient or outpatient setting, will occur about three times each week for at least two weeks.1
Repetitive Transcranial Magnetic Stimulation (rTMS)
Transcranial magnetic stimulation (TMS) is a procedure that works to stimulate nerve cells in the brain using magnetic fields. A magnet is placed on the forehead that releases pulses to the brain. The procedure is painless and can be placed on various parts of the head to target specific parts of the brain to improve depression.
For those with catatonic depression, TMS has shown to be effective as soon as after one session. Evidence suggests that patients are able to eat more, drink more water, and have better sleep. By the 10th session, TMS helped with improving both verbal and nonverbal communication as well.9
How to Get Help for Catatonic Depression
Getting help for catatonic depression differs from seeking help for other forms of depression, because when a catatonic period occurs, the person must rely on others. During catatonia, a person will require the intervention of friends, family, and loved ones to push for an accurate assessment and treatment. If a person begins to notice even a slight possibility that a catatonic episode is starting, they should take immediate action.
To slow the progression of catatonic depression, options include:
- Present to the nearest emergency room: catatonia is serious and may need inpatient psychiatric care as soon as possible to treat
- Contact a reliable prescriber: scheduling an appointment with a psychiatrist or nurse practitioner to occur soon could prevent catatonia from increasing its effects
- Phone a local crisis hotline: the negative impact of catatonia cannot be overstated, so crisis care is a good option. These hotlines can connect people to available services to quickly and effectively address symptoms.
In the case of other depressive disorders, a person can simply schedule an evaluation with a therapist and get on a waitlist for a prescriber, but this plan may develop too slowly.
How to Help a Loved One
Being the loved one of somebody with catatonic depression is an especially important role. The most important aspect here is to always approach your loved one from a position of love and support. Do not make threats, become defensive or judgmental, or give ultimatums as these can only aggravate symptoms. Have a conversation about risks, so you can feel confident in your decisions.
Here are practical ways to help a loved one with catatonic depression:
- Know the signs: since catatonic depression isn’t as common as other forms, it is a subtype of depression that is often misdiagnosed and misunderstood. Do some research to know the symptoms.
- Communicate your concern: a person should feel free and comfortable to speak openly with their loved one about the condition and the visible symptoms. Let them know what you are seeing and what you intend to do about it
- Know the options: you may be placed in the uncomfortable position of having to seek out emergency mental health services for your loved one. Learn about the options and how you can initiate a hospitalization if needed.
- Have a plan in place: once you have the options, finalize a plan with your loved one. With a plan in place, there will be less pressure and confusion when the symptoms emerge.
Depression Is Treatable With Therapy
Would you like to feel more happiness and joy? BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you.
5 Ways Cope With Catatonic Depression
Managing symptoms of catatonic depression requires healthy coping skills to mitigate the damaging effects. Coping skills act as protective factors that can prevent catatonic states from forming or lessen the severity of the condition when it emerges. The good news is that coping skills don’t need to be complicated, expensive, or demanding. Many are free and easily accessible.
Here are five coping strategies that work well for catatonic depression:7
- Maintain your treatment plan: it can be tempting to deviate from the plan by stopping medication or skipping therapy appointments, but these actions allow catatonic depression to come to the surface. Stick to the treatment plan. If questions arise, be sure to speak to your treatment team.
- Expand your support network: fighting catatonia alone is challenging because you may not be able to see the changes as they develop. Seek out new relationships in person and online to have a well-rounded network, and let them know the impact of depression in your life.
- Know what to avoid: many people, places, and things can trigger a period of depression, and knowing your triggers can provide unparalleled assistance. To begin, walk away from the negative coping skills like alcohol, drugs, unsafe sex, overspending, and other forms of distraction. These temptations only lead to increased symptoms.
- Focus on physical for mental: your mental health and physical health are closely tied, so focus on your physical to aid your depression. Adjusting your eating habits, exercise routine, and sleep schedule may lead to great results.
- Be patient: remember, positive coping skills, like healthy lifestyle changes, take time. Don’t fall victim to the quick fixes.
How to Deal With a Depressive Episode
Each day, it’s important to check in with your thoughts, feelings, and behaviors to see how they relate to depression. Even on good days, there could still be some depression present. Once you notice the symptoms, decide on a plan of action for what you should do about it. This is the time to assert your control.
Questions to consider:
- Do you want to call a friend or someone on your treatment team?
- Should you practice your at-home coping skills or therapeutic techniques given by your counselor?
- Do you need to seek emergency care?
Catatonic Depression Statistics
Catatonia is well-studied as an independent mental health condition and as one related to depression.
Some valuable catatonic depression statistics include:1,3,5
- Nearly 10% of people admitted to psychiatric hospitals are affected by catatonia
- Catatonia may occur with depression but about 20% of people with autism spectrum disorderASD will experience catatonia and up to 50% of catatonia cases are the result of medical issues
- About 80% of adults and 65% of children will report total alleviation of catatonic symptoms with lorazepam treatment
- Out of the 20% of adults who do not respond to lorazepam, 80% of those people will respond to ECT or a combination of ECT and lorazepam.
- Some forms of catatonia are related to mortality rates of around 10%, despite improving treatments
Final Thoughts on Catatonic Depression
If you or a loved one are dealing with catatonic depression, getting help is critical. While early intervention is best, it’s never too late to seek treatment.
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
Talk Therapy
Online-Therapy.com – Get support and guidance from a licensed therapist. Online-Therapy.com provides 45 minute weekly video sessions and unlimited text messaging with your therapist for only $64/week. Get Started
Online Psychiatry
Hims / Hers If you’re living with anxiety or depression, finding the right medication match may make all the difference. Connect with a licensed healthcare provider in just 12 – 48 hours. Explore FDA-approved treatment options and get free shipping, if prescribed. No insurance required. Get Started
Depression Newsletter
A free newsletter from Choosing Therapy for those impacted by depression. Get helpful tips and the latest information. Sign Up
Learn Anti-Stress & Relaxation Techniques
Mindfulness.com – Change your life by practicing mindfulness. In a few minutes a day, you can start developing mindfulness and meditation skills. Free Trial
Choosing Therapy Directory
You can search for therapists by specialty, experience, insurance, or price, and location. Find a therapist today.
For Further Reading
Online Depression Test A few questions from Talkiatry can help you understand your symptoms and give you a recommendation for what to do next. Best Online Psychiatry Services Online psychiatry, sometimes called telepsychiatry, platforms offer medication management by phone, video, or secure messaging for a variety of mental health conditions. In some cases, online psychiatry may be more affordable than seeing an in-person provider. Mental health treatment has expanded to include many online psychiatry and therapy services. With so many choices, it can feel overwhelming to find the one that is right for you.