Veterans often experience a variety of mental health concerns, including post-traumatic stress disorder (PTSD), traumatic brain injury (TBI), substance misuse, anxiety, depression, and suicidal ideation. Factors can include exposure to dangerous combat situations, deployments, injuries, military sexual trauma, relationship stress, reintegration into civilian life, and financial stress.
Recover From Trauma With The Help Of Therapist
Therapy can help you live a better life. BetterHelp provides convenient and affordable online therapy, starting at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you!
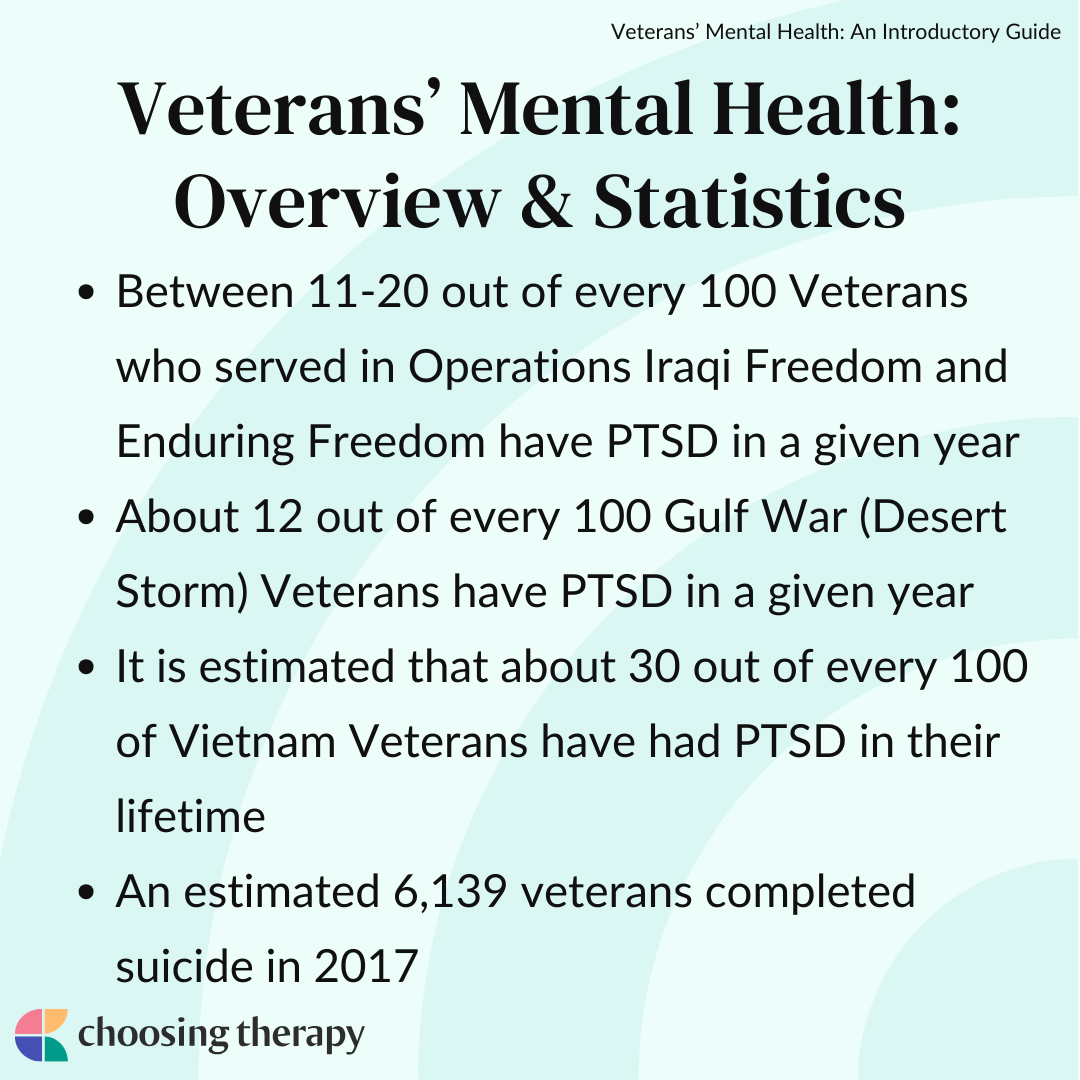
Veterans’ Mental Health: Overview & Statistics
According to the Veterans Affairs Office of Research and Development, in 2018 it was recorded that 1.7 million veterans received treatment through VA Mental Health specialty programs.1
Here are some statistics regarding veterans’ mental health:
- Between 11-20 out of every 100 Veterans who served in Operations Iraqi Freedom and Enduring Freedom have PTSD in a given year2
- About 12 out of every 100 Gulf War (Desert Storm) Veterans have PTSD in a given year2
- It is estimated that about 30 out of every 100 Vietnam Veterans have had PTSD in their lifetime2
- An estimated 6,139 veterans completed suicide in 20173
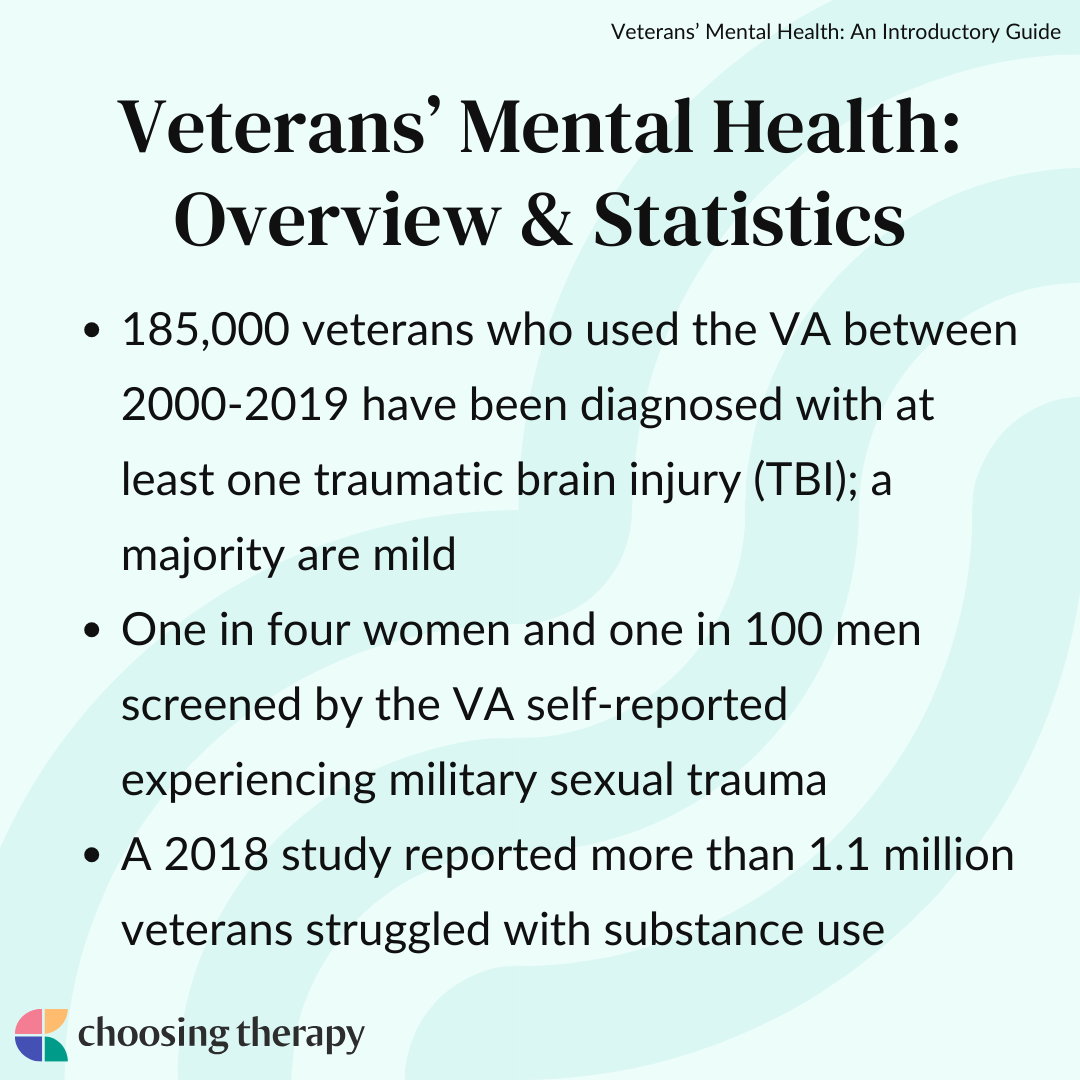
- 185,000 veterans who used the VA between 2000-2019 have been diagnosed with at least one traumatic brain injury (TBI); a majority are mild4
- One in four women and one in 100 men screened through the VA self-reported experiencing Military Sexual Trauma5
- A 2018 study reported more than 1.1 million veterans struggled with substance use6

“Many veterans struggle with PTSD, yet many of the veterans I see are dealing with major depression or anxiety due to other life challenges. These issues may range from relationship and marriage problems to difficulty transitioning to civilian life, as well as problems surrounding money and work.”
Veterans & PTSD
Post traumatic stress disorder (PTSD) is highly prevalent among veterans, especially combat veterans. Factors that increase the risk of PTSD in veterans can include what a service member does during the war, politics around the war, the location of the war, and the type of enemy a service member faces.2
Symptoms of PTSD can include:
- Experiencing nightmares and night terrors
- Reliving the event through PTSD flashbacks
- Avoidance of situations that remind you of the event
- Being easily startled or hyper-aroused
- Decreased interest in activities
- Withdrawing or isolating behaviors
- Increased anger or irritability
- Increased substance use or dependence
- Relationship strains
- Work issues
- Sadness
- Guilt
- Shame
Symptoms of PTSD can begin soon after a traumatic experience, develop later in life, or resurface again after a period of time. PTSD can increase with age for older veterans who experience medical problems, difficulty adjusting to retirement, or from watching, reading, or hearing about current wars.8
Online Therapy For PTSD Therapy can help you live a better life. BetterHelp provides convenient and affordable online therapy, starting at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you!
Veterans & Late-Onset Stress Symptomatology
Late-onset stress symptomatology (LOSS) can be experienced by veterans later in life as they age due to having more time, thoughts, and feelings about their military experience. LOSS can be triggered by age-related factors like retirement, the loss of loved ones, the death of fellow unit members, and health problems.
LOSS differs from PTSD because the contributing factors previously mentioned are all related to aging. Additionally, LOSS is not upsetting for every veteran, as some report it helps them connect their military experiences with making meaning in their current lives as they age.8
Veterans & Traumatic Brain Injuries
The Defense and Veterans Brain Injury Center (DVBIC) reported roughly 414,000 traumatic brain injuries (TBIs) among US service members between 2000 and 2019. TBIs can vary in severity and longevity.4 Veterans can experience headaches, irritability, vision or hearing issues, mood, focus, memory, physical functions, and impacts on relationships. Furthermore, veterans with TBIs have an increased risk of experiencing PTSD, anxiety, depression, substance use disorders, and sleep disturbances.4,9
TBIs and symptoms can further be complicated by the accumulation of multiple TBI events over the span of a person’s life. Research has indicated that there is a correlation between repetitive TBIs in combat veterans and chronic traumatic encephalopathy (CTE) and Parkinson’s disease.4
Veterans & Depression
Veterans are at a higher risk for developing depression.10,11 One study looked at the relationship between veterans and mental health issues and found that 1.15 million veterans were diagnosed with at least one mental health disorder, the most common being depression, substance use disorders, PTSD, and anxiety.10 Depression was the most prevalent of these conditions, at a rate of 13.5%.10
Additional research indicates that co-occurrence of depression and PTSD increases a veteran’s risk of suicidal ideation more than experiencing one of the conditions alone.11 Veterans sometimes experience combat-related guilt, and inappropriate or excessive guilt is a symptom of major depressive disorder, which may be compounded in this population.11
Veterans & Suicide
Suicide is a serious public health problem that impacts the entire nation, especially veterans. Additionally, suicide rates appear to be continuing to rise among veterans.6 One unique factor for veterans is the increased likelihood of owning or having easy access to firearms and the knowledge of how to use them.
Veterans are at an increased risk for suicide or suicidal ideation due to alarming rates of homelessness, unaddressed chronic health issues from military service, untreated mental health conditions, substance use disorders, difficulty reintegrating into civilian life, increased stress and relationship issues, sleep disturbances, and limited support networks.3
Veterans & Military Sexual Trauma
Military sexual trauma (MST) is not a diagnosis on its own, however, due to several unique factors it is important to mention that MST can have a profound impact on mental health. Unique factors can include a veteran continuing to reside, interact, or work with the perpetrator, belief that reporting will damage unit camaraderie or spirit, belief of appearing vulnerable or weak among colleagues, and fear of being excluded for further promotions.12
MST symptoms can include:13
- Experiencing difficult memories
- Nightmares and sleep disturbances
- Feeling unsafe or numb
- Increased use of substances
- Feelings of depression
- Anxiety
- Isolation
- Feeling irritability or increased anger
- Aversion to touch
- Questioning or doubting self
- Sexual or physical health problems
Symptoms resulting from sexual trauma can be delayed and may not surface until months, years, or after leaving military service.
Most people don’t understand. Therapists do. Therapy can help you overcome trauma from sexual assault. BetterHelp provides convenient and affordable online therapy, starting at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you!
Veterans & Substance Abuse
Substance use disorder among veterans can occur for a variety of reasons. Some veterans use substances to cope with mental health issues like trauma exposure, depression, anxiety, and reintegration stress. Others might develop a substance use issue after injury or to manage pain symptoms. According to research, illicit drug use increases when leaving military service due to no longer participating in random drug screens.14
A 2018 study reported more than 1.1 million veterans struggled with substance use. The same study highlighted the following statistics:6
- 1 in 4, or about 300,000, reported struggling with illicit drugs
- 4 in 5, or about 899,000, struggled with alcohol use
- 1 in 13, or about 78,000, struggled with both illicit drug and alcohol use
- The most common illicit drug use is marijuana
One complication among those with substance use disorders is the prevalence of co-occurring mental health issues like depression, anxiety, bipolar disorder, and other serious mental health diagnoses. Untreated mental health conditions can be exacerbated by substance use. Also, substance use can be exacerbated by untreated mental health conditions as a way to cope and self-manage symptoms.
Veterans with substance use disorders are 3-4 times more likely to be diagnosed with PTSD or depression diagnosis from a mental health professional.14 It is important to seek treatment where both issues of substance use and mental health can be addressed, if possible, to receive the best possible care.
Barriers to Treatment as a Veteran
Barriers to treatment impact veterans for various reasons, including issues with transportation or not knowing their care and benefit options. They may also be concerned about losing job security or other opportunities if they seek care.
A 2018 evaluation of VA mental health services reported the following common barriers to treatment for veterans:15
- Lack of knowledge on how to apply for benefits
- Misunderstanding eligibility due to certain qualifying factors that determine the level of care and benefits
- Transportation challenges
- Long distances from available VA care
- Limited or no access to public transportation to receive care
- Employment concerns
- Requesting time off of work
- Fear of impact on security clearance
- Unable to arrange childcare
- Judgment from colleagues
- Scheduling Issues
- Lack of flexible scheduling
- Long wait periods between appointment requests and scheduling
Dr. Carlos Garcia shares, “I believe the other greatest obstacle has to do with the ongoing stigma around getting therapy. Veterans often express their concern over stigmatizing labels as well as military attitudes fostering feelings of weakness and failure. Unfortunately, this leads to many veterans assuming they are not ‘sick enough’ to get therapy because their situation is ‘not that bad.’”
The Stigma of Getting Help as a Veteran
It is important to point out that the military has its own separate cultural identity and norms within the system. This creates dynamics and cultural influences within the armed services that directly impact barriers to services. There is a mental health stigma that can create fear, shame, and embarrassment to seek services.

“Veterans are accustomed to hardship, to privation, to going without. They embrace the slogans so associated with Service: ‘Suck it up.’ ‘Drive on.’ ‘March or die.’ From here, it is an easy step to translate “seeking help” into the language of one who failed to persevere through trial, who “caved,” who had to ask for help, and who couldn’t finish on their own. There is no shame in asking for help. But Veterans are not only a durable lot—they are a proud lot, as well. Oddly, they may often seek help in other matters, but not mental health.”
Who Should I Tell About My Mental Health Concerns?
It is important for you to develop a treatment team and support system around your mental health concerns. An integrated mind, body, and soul approach to recovery from symptoms can help you attend to your needs. Seeking the care of a primary care provider for physical health, a therapist for mental health, and the support of a community clinic may be good resources to start.
Help For Trauma / PTSD
Talk Therapy – Get help recovering from trauma from a licensed therapist. Betterhelp offers online therapy starting at $60 per week. Free Assessment
Online PTSD treatment – Talkiatry offers personalized care from psychiatrists who listen and take insurance. Get matched with a specialist in just 15 minutes. Take our assessment
Will Asking for Help Affect My Career?
You can’t be fired for your mental health concerns, and there are laws preventing employers from asking questions about your mental or physical health conditions or using this information against you. On another note, some employers may actually value you sharing about your condition and find this as a point of connection and personability. Additionally, it can be more harmful to your career for mental health conditions to go undiagnosed and untreated, as they can impact your motivation and ability to perform.
How Therapy Can Help Veterans Improve Veterans’ Mental Health
Therapy can create a space to promote a better understanding of experiences, feelings, and behaviors in a safe and controlled environment. Veterans can learn strategies to manage and cope with their mental health and build a strong support network.
Dr. Carlos Garcia shares, “There is nothing more powerful for healing than sharing our stories. It helps veterans to find the root cause of their problem while finding solutions to address those challenges. Therapy helps veterans to better understand their inherent strengths and to use those strengths to improve their lives. Therapy also helps veterans see that going to therapy does not mean we are ‘weak,’ but instead that we are brave for facing our challenges head on.”
Here are some other benefits of therapy for veterans, according to Steven Berry:
- Redefine expectations: Veterans are, by nature, “fixers.” We want to fix it. We can “make it happen.” However, in the more delicate matters involving the soul and the mind, this attitude is often unhelpful at best and, at worst, harmful and detrimental. Helping Veterans manage their own expectations about treatment protocols and what progress might look like is helpful.
- Enable a proper understanding of “resilience”: Resilience, simply put, is the ability to bounce back from traumatic experiences to return to a normal state after being distorted or exposed to stress. It’s not that someone should expect to be unaffected by stress—in this case, the stresses of combat—but that they can be restored after experiences.
- Receive objective, dispassionate input: Most veterans are so deeply engaged with their issues or with what they think/perceive as their issues that we can see only trees and no forest at all. The value of an objective, dispassionate counselor who can properly employ a well-chosen therapeutic approach geared toward the Veteran at hand cannot be understated.
Finding a Therapist Who Understands Veterans’ Concerns
Therapy is a deeply personal experience, and it is important to find a therapist who can address your needs and make you feel comfortable engaging in treatment.
A few helpful questions to consider while seeking out service can include:
- Do I prefer one-on-one counseling or group counseling?
- Would I feel more comfortable speaking to a therapist who has military experience?
- How important is it for my therapist to have experience working with veterans?
- What kind of specialities would I like my therapist to have?
- PTSD, depression, anxiety, a trauma-informed lens?
Recover From Trauma With The Help Of Therapist
Therapy can help you live a better life. BetterHelp provides convenient and affordable online therapy, starting at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you!
Mental Health Resources Available to Veterans & Their Families
Mental health is an important factor to overall health and wellness for veterans. The increased understanding of the importance of providing mental health resources for veterans has created a multitude of options for mental health care. Veterans can seek resources through government funded agencies, private sector care like psychiatric hospitals or specialized individual mental health providers, and non-profit agencies that specifically work with veterans and their families.
Mental health resources available to veterans and their families include:
- U.S. Department of Veterans Affairs
- Military One Source
- Helping Out Our American Heroes
- Wounded Warrior Project
- Vets 4 Warriors (*Peer Consultants)
- Fisher House
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- or call 800-662-4357
- National Suicide Prevention Lifeline
- or call 800-273-8255 Veterans can press 1
- Options For Deaf + Hard of Hearing For TTY Users: Use your preferred relay service or dial 711 then 1-800-273-8255.
- Make the Connection
How to Support a Veteran Experiencing Mental Health Concerns
Steven Berry compiled a list of helpful tips for supporting a veteran:
- Be patient: Some things about your veteran have changed. It is unrealistic to think otherwise. Life experiences change us. Exposure to the stresses of combat changes us, sometimes in ways for our own good and for the good of others. Some things that are learned become “hardwired” and may be impossible to unlearn. Destructive behaviors are another matter, and they should be dealt with otherwise. Substance abuse, domestic violence, and the like cannot be excused. They must be confronted, often by intervention.
- Practice loving insistence: Sometimes it is best to have your say and, having done so, to give it a rest. Remember, you don’t need to attend every argument to which your veteran invites you.
- Do not enable the Veteran: Codependent behaviors on the part of family members are not helpful.
- Do not make excuses for the Veteran: Do not make excuses for your veteran’s actions or inactions. Avoid the temptation to rescue and to make excuses. Your veteran’s accountability is an important component of their restoration and/or recovery.
- Find your own “Tribe:” You are not alone. There are others out there who are just like you and who have real struggles and adjustments just like you. Find someone, or a group of people, in whom you can confide, in whom you can trust, someone who will safeguard your concerns (with a couple of possible exceptions), someone who will not judge either you or your veteran.
- Practice good self-care: Identify some things to do for yourself to disengage for brief times. Step away from the fray. Get a pedicure. Take a walk. Join a yoga class. Explore the possible benefits of counseling for yourself. Find a support group.
- Give your veteran some space: This is especially true for spouses and family members of male veterans, I think. John Gray has written about men and their desire to spend time alone in “the cave.” Respect your male veteran’s “cave time.” Good things can happen in the cave. Restorative things can occur there. The cave is not a place to live but to re-group, to re-invigorate.
- Understand relapse: Along the road to healing, most veterans will relapse with or into something. For substance users, relapse is a real possibility. The depression that may follow alcohol cessation may contribute to relapse. An event or particular anniversary (death of a Comrade, a hard fight, a terrifying experience, a particular smell) may contribute to a relapse. Relapse is not equal to ruin. It is part of the struggle, and it’s possible to come up with effective relapse prevention strategies.
Knowing the Mental Health Warning Signs for a Loved One Transitioning to Civilian Life
Knowing mental health warning signs can help you watch out for your loved one as they are making the transition back into civilian life. This period can be a higher risk and vulnerable time for a veteran, as they navigate new challenges unrelated to the type of life they are used to. Knowing the signs of an impending crisis can help you encourage your loved one to seek early intervention.
Warning signs of a mental health crisis or concern include:
- Rapidly shifting emotional states
- Increased aggression or irritability
- Trouble falling or staying asleep
- Seeing, hearing, or perceiving things that are not there
- New or increased use of drugs or alcohol
- Frequent fights with those around them
- Absences from work or functions
- Long periods of isolation
In My Experience
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
Online Therapy
BetterHelp – Get support and guidance from a licensed therapist. BetterHelp has over 25,000 therapists who provide convenient and affordable online therapy. Take A Free Online Assessment and get matched with the right therapist for you. Free Assessment
Online PTSD treatment
Talkiatry offers personalized care from psychiatrists who listen and take insurance. Get matched with a specialist in just 15 minutes. Take our assessment.
Treatment For Trauma & OCD
Half of people diagnosed with OCD have experienced a traumatic life event. The chronic exposure to stressful situations, such as ongoing bullying, or an abusive relationship can lead to the development of OCD symptoms. NOCD therapists specialize in treating both trauma and OCD and are in-network with many insurance plans. Visit NOCD
Trauma & Abuse Newsletter
A free newsletter for those impacted by trauma or abuse. Get encouragement, helpful tips, and the latest information. Sign Up
Choosing Therapy Directory
You can search for therapists by specialty, experience, insurance, or price, and location. Find a therapist today.
How Does ERP Help With Intrusive Thoughts? Obsessive compulsive disorder (OCD) is a psychiatric condition marked by the presence of obsessive thoughts, images, doubts, or urges, followed by compulsive behaviors or acts aimed at easing the distress caused by the obsession. While the content of the obsessions can take many forms, they are always repetitive, persistent, involuntary, and intrusive, and they often result in a great deal of anxiety for the person experiencing them. 9 Types of Therapy for Trauma Experiencing trauma can result in distressing and debilitating symptoms, but remind yourself that there is hope for healing. If you or a loved one is suffering from the aftereffects of trauma, consider seeking therapy. Trauma therapy can help you reclaim your life and a positive sense of self. 
Choosing Therapy strives to provide our readers with mental health content that is accurate and actionable. We have high standards for what can be cited within our articles. Acceptable sources include government agencies, universities and colleges, scholarly journals, industry and professional associations, and other high-integrity sources of mental health journalism. Learn more by reviewing our full editorial policy.
-
US Department of Veterans Affairs. Mental Health. https://www.research.va.gov/topics/mental_health.cfm.
-
US Department of Veterans Affairs (2018, July 24) PTSD: National Center for PTSD. How Common is PTSD in Veterans? https://www.ptsd.va.gov/understand/common/common_veterans.asp.
-
US Department of Veterans Affairs. Suicide Prevention. Office of Research & Development. https://www.research.va.gov/topics/suicide.cfm.
-
Department of Veterans Affairs. Traumatic Brain Injury (TBI). Office of Research & Development. https://www.research.va.gov/topics/tbi.cfm.
-
US Department of Veterans Affairs (2019, October 17) PTSD: National Center for PTSD. Military Sexual Trauma. https://www.ptsd.va.gov/understand/types/sexual_trauma_military.asp
-
Substance Abuse and Mental Health Services Administration U.S. Department of Health and Human Services. (2020, January 14). 2018 National Survey on Drug Use and Health: Veterans. https://www.samhsa.gov/data/sites/default/files/reports/rpt23251/6_Veteran_2020_01_14_508.pdf
-
Garcia, Carlos. (2021). Personal Interview.
-
US Department of Veterans Affairs (2007, January 1) Aging Veterans and Posttraumatic Stress Symptoms. PTSD: National Center for PTSD. https://www.ptsd.va.gov/understand/what/aging_veterans.asp.
-
US Department of Veterans Affairs. (2018, November 29). Effects of TBI. Mental Health. https://www.mentalhealth.va.gov/tbi/index.asp.
-
Trivedi, R. B., Post, E. P., Sun, H., Pomerantz, A., Saxon, A. J., Piette, J. D., Maynard, C., Arnow, B., Curtis, I., Fihn, S. D., & Nelson, K. (2015). Prevalence, Comorbidity, and Prognosis of Mental Health Among US Veterans. American journal of public health, 105(12), 2564–2569. https://doi.org/10.2105/AJPH.2015.302836
-
Sher, L., Braquehais, M. D., & Casas, M. (2012). Posttraumatic stress disorder, depression, and suicide in veterans. Cleveland Clinic journal of medicine, 79(2), 92. https://web.archive.org/web/20190302203149id_/http://pdfs.semanticscholar.org/a1b4/dfecc3813c4b582fb6e09ea0cec7879e7814.pdf
-
Make the Connection. Effects of Military Sexual Trauma. https://www.maketheconnection.net/conditions/military-sexual-trauma/.
-
US Department of Veterans Affairs. (2010, April 14). Military Sexual Trauma. Mental Health. https://www.mentalhealth.va.gov/msthome/index.asp.
-
National Institute on Drug Abuse NIDA. 2019, October 23. Substance Use and Military Life DrugFacts. https://www.drugabuse.gov/publications/drugfacts/substance-use-military-life.
-
Evaluation of the Department of Veterans Affairs Mental Health Services. (2018). National Academies Press.

We regularly update the articles on ChoosingTherapy.com to ensure we continue to reflect scientific consensus on the topics we cover, to incorporate new research into our articles, and to better answer our audience’s questions. When our content undergoes a significant revision, we summarize the changes that were made and the date on which they occurred. We also record the authors and medical reviewers who contributed to previous versions of the article. Read more about our editorial policies here.
Author: Ashley Stuck, LCSW (No Change)
Medical Reviewer: Benjamin Troy, MD (No Change)
Primary Changes: Fact-checked and edited for improved readability and clarity.
Author: Ashley Stuck, LCSW (No Change)
Medical Reviewer: Benjamin Troy, MD (No Change)
Primary Changes: Added sections “Veterans & Depression”, “Who Should I Tell About My Mental Health Concerns?”, “Will Asking for Help Affect My Career?”, “Knowing the Mental Health Warning Signs for a Loved One Transitioning to Civilian Life”. New material written by Christina Canuto, LMFT-A and reviewed by Kristen Fuller, MD. Fact-checked and edited for improved readability and clarity.
Author: Ashley Stuck, LCSW
Reviewer: Benjamin Troy, MD

Your Voice Matters
Can't find what you're looking for?
Request an article! Tell ChoosingTherapy.com’s editorial team what questions you have about mental health, emotional wellness, relationships, and parenting. The therapists who write for us love answering your questions!
Leave your feedback for our editors.
Share your feedback on this article with our editors. If there’s something we missed or something we could improve on, we’d love to hear it.
Our writers and editors love compliments, too. :)