Opioid use disorder treatments are available to help people overcome dependence and achieve sobriety. Therapy can help those struggling with opioid addiction identify the reasons for their addictive behavior, while medications like buprenorphine and methadone can reduce withdrawals and cravings.
What Are Opioids?
Opioids are medications prescribed to treat pain. While these painkillers can help alleviate chronic pain, opioids are highly addictive and dangerous when misused.1 Opioids are highly addictive, quickly resulting in physical dependence and tolerance.2
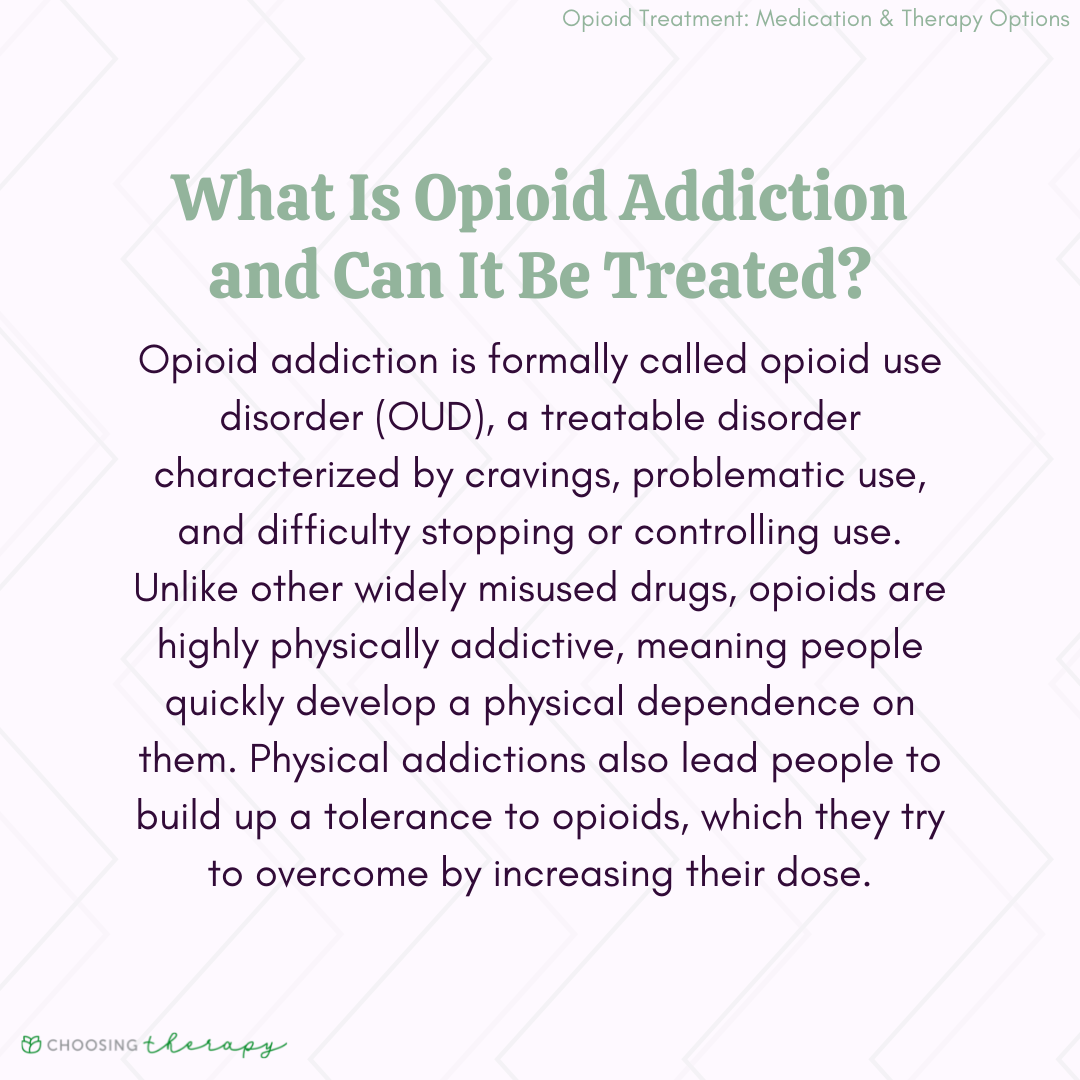
What Is Opioid Use Disorder?
Opioid use disorder (OUD), informally known as opioid addiction, is a treatable disorder characterized by problematic use of opioids.2 People with OUD experience intense cravings for the drug and struggle to stop using. Abusing prescribed or illicit opioids, such as heroin, can result in dependence, withdrawal, overdose, and death.1,2
Workit Health - Online Treatment for Opioids or Alcohol, Including Medication. Modern, personalized recovery that combines medication, a supportive community, and helpful content. Covered by many insurance plans. Currently available in FL, TX, OH, MI, and NJ. Learn more
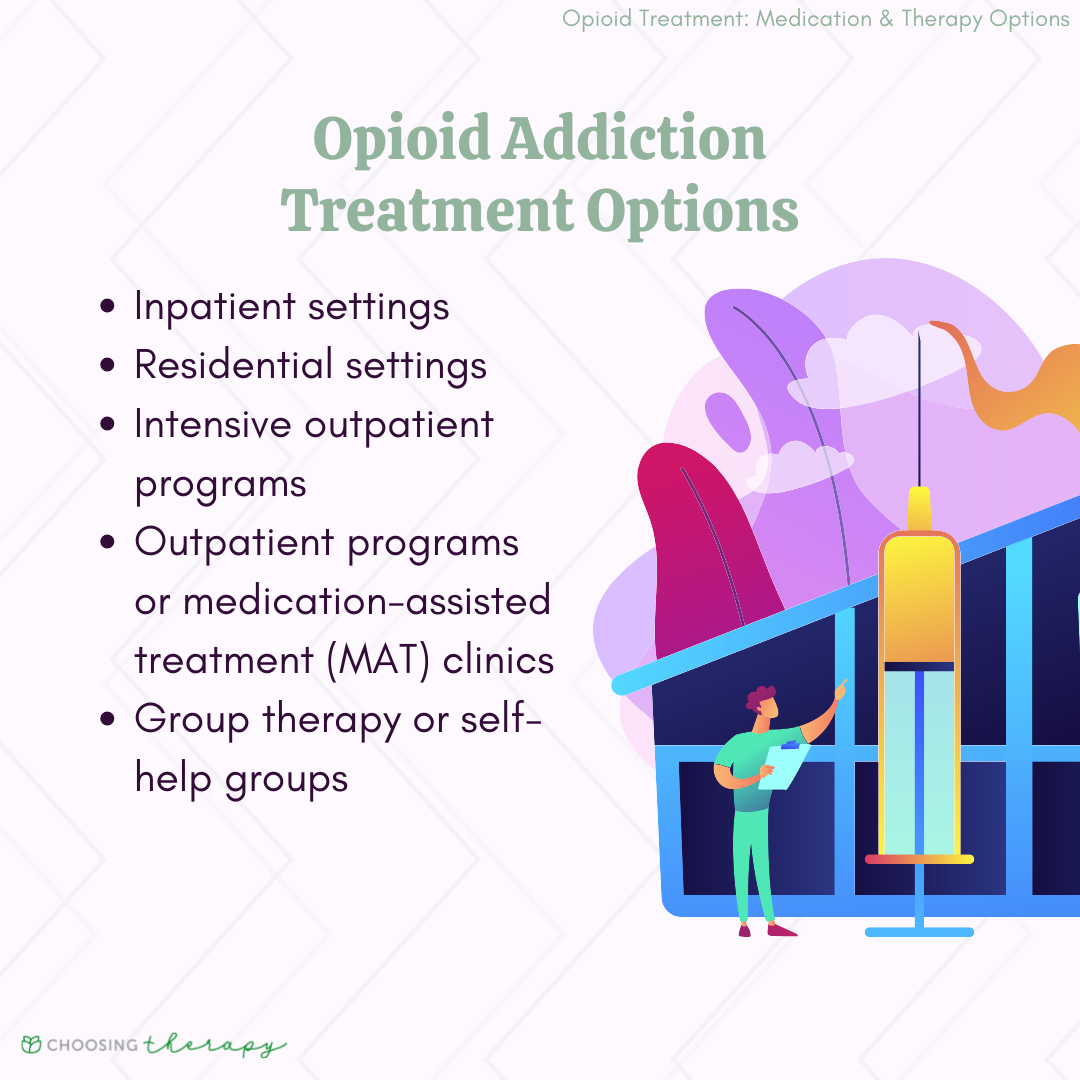
Opioid Addiction Treatment Options
Opioid addiction treatment exists in both inpatient and outpatient forms. Rehab facilities focusing on treatment for opioid use disorder often include a combination of medication and therapy. The type of treatment a person receives depends on several factors, including the severity of their dependency, risk of relapse, and ability to afford treatment.3
Medication-Assisted Treatment (MAT) for Opioid Addiction
When treating opioid use disorder, many clinicians consider medication-assisted treatment (MAT) a frontline option for opioid use disorder. Inpatient or outpatient rehab centers may provide MAT with cognitive behavioral therapy (CBT), motivational interviewing, and other therapeutic elements.3
Opioid addiction medications used in treatment can include:
Methadone
Methadone is a prescription opioid only administered by SAMHSA opioid treatment programs (OTP). Methadone attaches to opioid receptors in the brain to block withdrawal and cravings. Adverse effects may include weight gain, drowsiness, or constipation. Addiction and dependence are possible when taking methadone.
Complications of methadone in opioid use disorder treatment are relatively low when individuals take the medication as prescribed. However, those who combine methadone with other substances or medications are at risk of severe drug interactions. To help prevent misuse, people must receive their prescriptions from certified SAMHSA OTP clinics.
Buprenorphine
Buprenorphine works by binding with opioid receptors to reduce cravings and withdrawal. Individuals may take the medication as a tablet, dissolvable film, or monthly injection. Common side effects include drowsiness, brain fog, constipation, and headaches.
Buprenorphine may be self-administered at home. However, like methadone, buprenorphine can be addictive, and individuals may experience withdrawal when they cease buprenorphine treatment or taper doses.
Naltrexone
Naltrexone blocks opioid receptors in the brain, preventing the pleasurable effects of opioids. In treatment for opioid addiction, naltrexone helps prevent relapse after someone has already experienced opioid withdrawal. Naltrexone is a non-addictive monthly injection, and patients can stop naltrexone treatment without experiencing withdrawal symptoms. Always consult with a doctor before stopping medication during opioid addiction treatment.
Lofexidine
Lofexidine is an as-needed opiate addiction medication that attaches to adrenergic receptors in the brain to help alleviate withdrawal symptoms. Lofexidine was formally an off-label medication for opioid use withdrawal before being FDA-approved for OUD in 2018. Lofexidine is not habit forming and has relatively mild adverse effects, which can include hypotension, dizziness, sleepiness, and dry mouth.
Naloxone
Naloxone (Narcan) is an emergency medication used to reverse symptoms of an overdose. Alternatively, naloxone can be added to buprenorphine to lessen the euphoric effects of an opioid. Naloxone is a life-saving drug when administered quickly.
Residential Opioid Use Disorder Treatment
Residential rehab centers for opioid use disorder offer 24-hour live-in facilities where clients engage in individual and group therapy, medication management and other interventions. Many residential facilities aim to provide a home-like, substance free environment that is safe, healthy and welcoming. Peer support is a key factor in the residential treatment model, as clients support one another along their journey toward sobriety.
Residential treatment for opioid addiction has been shown to have positive outcomes, particularly in enhancing recovery-related functioning in the short-term.4 However, there is limited evidence that residential opioid use disorder treatment is any more effective than less intensive approaches.5 Of all opioid addiction treatment options available, residential treatment is by far the most expensive, and some studies have raised concerns about the quality of care provided by residential treatment programs.6
Workit Health - Online Treatment for Opioids or Alcohol, Including Medication. Modern, personalized recovery that combines medication, a supportive community, and helpful content. Covered by many insurance plans. Currently available in FL, TX, OH, MI, and NJ. Learn more
Intensive-Outpatient Treatment for Opioid Addiction
Intensive-outpatient treatment offers similar addiction help to what is available in a residential treatment facility, however the client remains in their own home and participates in individual and group therapy several times a week, along with medication management. This intervention, also sometimes referred to as partial hospitalization, offers more intensive therapeutic intervention, with sessions often meeting several times a week for several hours at a time.
In terms of opioid treatment programs, the intensive-outpatient approach is the most commonly used and widely available. While pharmacological interventions have been shown to be the most promising in helping people facing opioid addiction, residential and intensive-outpatient treatment options are valuable supplements to medication.7
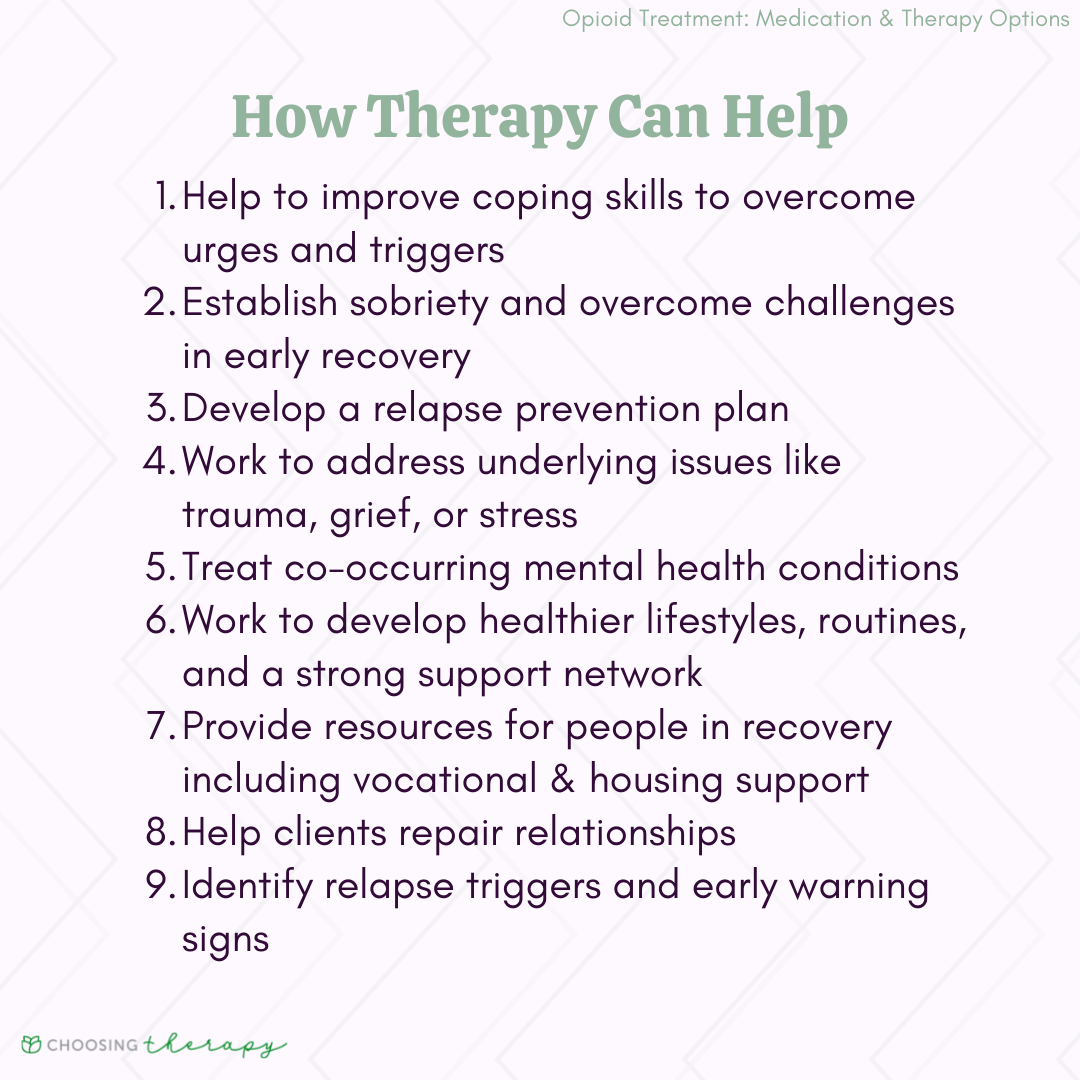
Opioid Use Disorder Therapies
Therapy for opioid addiction is an essential aspect of recovery and long-term success. The goals of opioid use disorder treatment depend on the individual but generally focus on improving coping skills, establishing sobriety, and treating co-occurring mental health conditions. Therapists can also help clients develop a relapse prevention plan and support network to improve the chances of long-term recovery.
An online therapist directory can help you choose a therapist with credentials to back up their experience.
Therapies in opioid use disorder treatment may include:
- Cognitive behavioral therapy (CBT): CBT for addiction helps clients to restructure their thought patterns in order to live a healthier life. It has been shown to be more effective than standard methadone drug counseling in reducing opioid use in patients enrolled in methadone maintenance treatment programs.8
- Family therapy: Family therapy can often be an important part of opioid use disorder treatment, and may include behavioral contracting to create a written plan for creating a substance-free home environment. Support from family and friends is an important part of recovering from opioid addiction.
- Motivational interviewing: This collaborative, nonjudgmental approach motivates the client toward positive change in alignment with the client’s own values and goals. One study found that a motivational interviewing treatment approach reduced opioid overdose rates in clients receiving the intervention.9
- Contingency management: This behavioral intervention rewards positive behaviors, and has been shown to be effective in reducing opioid use.10
- Group therapy: Regularly meeting with peers facing similar challenges in a group therapy setting can provide a meaningful and effective supplement to other interventions. One particular group intervention known as mindfulness-oriented recovery enhancement (MORE) has been shown to be a useful complementary treatment for people facing opioid use disorder.11
Final Thoughts
Opioid addiction treatment can help you overcome OUD. While a ‘one-size-fits-all’ solution for opioid addiction does not exist, various programs and therapists can work with you on creating a unique treatment plan. Addressing the root issues behind your opioid use and building healthy routines aid recovery.
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below. Online Treatment for Opioids or Alcohol, Including Medication. Workit Health – Modern, personalized recovery that combines medication, a supportive community, and helpful content. Covered by many insurance plans. Currently available in FL, TX, OH, MI, and NJ. Visit Workit Health Alcohol Treatment – Cut Back or Quit Entirely Ria Health – Quickly change your relationship to alcohol with our at-home program. On average, members reduce their BAC levels by 50% in 3 months in the program. Services are covered by many major health plans. Visit Ria Health Drug Addiction Rehab Centers Recovery.com – Find the best local detox or drug rehab center covered by your health insurance. Search by location, condition, insurance, and more. Read reviews. Start Your Search Telehealth Treatment For Opioid Use Disorder Bicycle Health – offers therapy, support, and medication for addiction treatment (MAT). MAT offers the lowest relapse rates for opioid use disorder, helping people to stop using opioids with minimal physical discomfort. Covered by most major insurance. Visit Bicycle Health Drinking Moderation Sunnyside – Want to drink less? Sunnyside helps you ease into mindful drinking at your own pace. Think lifestyle change, not a fad diet. Develop new daily routines, so you maintain your new habits for life. Take a 3 Minute QuizAdditional Resources
Best Online Medication-Assisted Treatment Programs Online medication-assisted treatment programs are fairly new to the telehealth industry, but existing companies are expanding quickly with new programs emerging every day. It’s important to explore your options and understand the level of virtual care available so you can choose the best addiction treatment program for you.
Best Mindful Drinking Apps If you’re thinking about joining the sober curious movement and you’d like to cut back on drinking, mindful drinking apps are a great place to start. Practicing mindful drinking can take some time, attention, and patience, but with the help of the right app, you can completely transform your relationship with alcohol.