OCD and depression are mental health conditions that share overlapping symptoms, such as struggling with intrusive thoughts, poor self-esteem, and loneliness. Due to these similar experiences, those with OCD may also develop depression at some point in their life. Despite this association, these disorders are two very different diagnoses.
Depression & OCD Treatment
Exposure And Response Prevention Therapy (ERP) – Do live video sessions with a therapist specialized in ERP, the gold standard treatment for OCD. Treatment from NOCD is covered by many insurance plans. Start With A Free 15 Minute Call
What Is Depression?
Depression is a common mental health disorder that includes symptoms such as a loss of energy, disinterest in normal activities, hopelessness, and increased irritability.1 Someone with depression may also experience less observable behavioral changes, making it difficult for others to recognize signs of the condition. According to the DSM-5TR, there is a difference in diagnosable depression and general sadness. While sadness is a normal human experience, depression involves a low mood that has persisted for at least two weeks.2
Common symptoms of depression include:
- Irritability or changes in mood
- Changes in sleep or inability to sleep
- Loss of appetite
- Low self-esteem and poor feelings of self-worth
- Difficulty concentrating, making decisions, or performing daily routines (like proper hygiene)
- Hopelessness, intense sadness, or melancholy
- Poor thoughts about the present or future
- Frequent thoughts about death, dying, or even suicide
What Is OCD?
Obsessive compulsive disorder (OCD) is characterized by obsessions and compulsions. Compulsions are thoughts or behaviors that are created as a response to unwanted, intrusive thoughts (obsessions). The DSM-5TR describes compulsions as being repetitive or ritualistic, and are performed to “neutralize” or soothe anxiety.2
Is There a Link Between Depression & OCD?
Due to the potentially distressing nature of OCD, it is common for depressive symptoms to also occur and impact someone’s ability to function.3 Seeing as avoidance, anxiety, and fear are characteristic emotional traits of OCD, it is understandable that a person with OCD may become sad about the quality of their life.
Certain negative or pessimistic views of oneself can easily translate into negative thoughts or hopelessness about the future.3 Therefore, it is likely that a person with OCD may develop a co-occurring depressive disorder. The comorbidity rate of these two disorders is quite high, as about half of those with diagnosable OCD also meet criteria for major depressive disorder.4
Can Depression Cause OCD?
Current research suggests that depression does not cause OCD. The cause of OCD is not definitively known, however research points to several known risk factors.
Risk factors for OCD include:11,12
- Having an immediate family member with OCD
- Differences in the brain’s frontal cortex and subcortical structures
- Childhood trauma
- Streptococcal infection
Can OCD Cause Depression?
OCD is not a direct cause of depression, but it can play a role in the development and persistence of depressive symptoms. For instance, when someone experiences frequent, intrusive thoughts that take up a significant amount of their time, they may lose out on opportunities that maintain a healthy mindset, such as social or physical activities.
Additionally, someone with OCD can have “bouts” of triggers followed by response behaviors, similar to the experience of “bouts” of depression. When these strike unexpectedly, the development of depressive symptoms can follow, especially if the OCD is triggered by trauma, stress, or abuse.5
Obsessions & Depression
Intrusive thoughts can cause significant distress, often leading to poor self-esteem, or even disgust with themself and their thoughts. It is common for those with OCD to feel angry about having their obsessions, wishing the thoughts would go away.
A person’s level of insight into the legitimacy of these obsessions may also play a role in how much distress it causes them. For example, someone may understand and recognize that their OCD obsessions are extreme and irrational. Another person might truly believe they are causing harm to others by not performing their ritualized behavior to stop something bad from happening. This level of anxiety and worry about harm to themselves or others can induce intense feelings of guilt and shame. In turn, depressive symptoms may develop.
Compulsions & Depression
Compulsions can look like repetitive hand washing, putting things in a specific order, or repeated checking.2 They can also include thought-based or mental acts such as praying, counting, or repeating words to oneself silently.2
People with OCD may also be perfectionistic, applying rigid rules to themselves and their behaviors. By going above and beyond to put their world back in order, they might believe they can prevent something bad from happening. As having control over many circumstances is not guaranteed, it is common for a person with OCD to become depressed or hopeless about the future.
Depression Related to Ability to Function
Intrusive thoughts and compulsions can inhibit a person’s ability to function in daily life. In fact, studies have shown that, compared to milder forms of OCD, the more severe obsessions and compulsions are, the more they interfere with daily functioning, leading to worsening depressive symptoms.13 As intrusive thoughts and compulsive rituals interfere with a person’s schedule, they are less able to keep up with daily responsibilities, such as personal hygiene, caring for their home environment, fulfilling work commitments, and spending time on hobbies and interests.
Impacts on Relationships
OCD affects a person’s life in many ways, but the potential loss of relationships can be so anxiety-provoking for some that they start to shut down and internalize these fears. For those with OCD, it can be difficult to ask for help or engage with other people, especially if social engagement is at the root of their fears. For example, those who obsessively worry about contamination are likely going to avoid other people.
OCD, Anxiety, & Depression
If OCD continues without being addressed, anxiety symptoms can manifest and lead to other issues like depression. Untreated anxiety can have major, long-term effects on the brain and impact areas of memory, attention, and executive functioning.6 Additionally, guilt commonly associated with anxiety disorders can result in the development of depressive symptoms, such as low self-worth and poor self-esteem.7
Treatment For OCD NOCD: Online OCD Treatment Covered By Insurance – Regain your life from OCD. Do live video sessions with a licensed therapist specialized in treating OCD. Treatment from NOCD is covered by most major insurance plans. Learn how you can use your insurance benefits. Visit NOCD Talkiatry: Is OCD Medication Right For You? Speak with A Doctor – Talkiatry can match you with a psychiatrist who takes your insurance and is accepting new patients. They’re in-network with major insurers and offer medication management with supportive therapy. Free Assessment
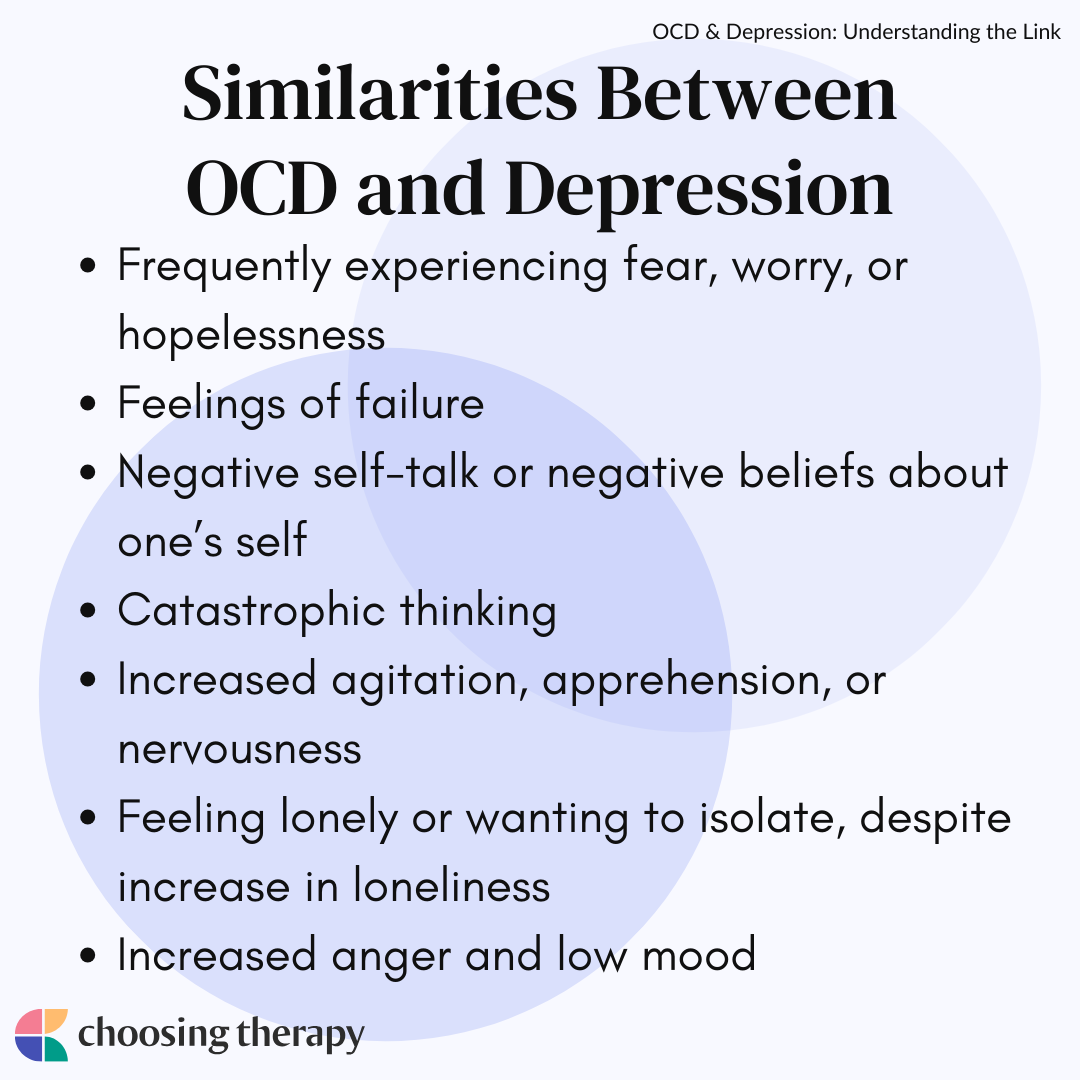
Similarities Between OCD & Depression
Both OCD and depression can include a fixation on unhelpful, negative thoughts that are often about the future or one’s inability to control the present.8 From a biological perspective, the amygdala (the part of the brain responsible for emotional processing) responds to overactive levels of distress, producing similar symptoms.9
OCD and depression share many overlapping symptoms, including:
- Frequently experiencing fear, worry, or hopelessness
- Feelings of failure
- Negative self-talk or negative beliefs about oneself
- Catastrophic thinking
- Increased agitation, apprehension, or nervousness
- Feeling lonely or wanting to isolate, despite increase in loneliness
- Overall poor life-satisfaction
- Increased anger and low mood
OCD Vs. Depression
Although similar, the two disorders are distinct: OCD is ritualistic, repetitive, and patterned whereas depression is more generalized. While intrusive, ruminating thoughts are a hallmark trait of both OCD and depression, those with OCD will experience these at an excessive, extreme frequency compared to those with depression—and respond with specific compulsive behaviors.8
Some differences between OCD and depression include:
- Frequency and intrusiveness of thoughts: While those with depression experience thoughts that are common to them, a person with OCD experiences repetitive thoughts until something is done about them.
- The presence of compulsions in OCD: While someone with depression may say their negative thoughts don’t let up, they don’t respond to them with compulsions in the same way people with OCD must complete an action in response to their intrusive thoughts.
- OCD-related disorders: The DSM-V suggests that body dysmorphic disorder, hoarding disorder, trichotillomania (hair-pulling disorder), and excoriation (skin-picking) disorder are OCD-related disorders (not caused by OCD).
- OCD can be a predictor of depression: There is a high chance someone with OCD might experience depression but depression itself cannot “cause” OCD.
Do I have OCD? The first step to getting help is an accurate clinical assessment and diagnosis. NOCD’s therapists will provide a comprehensive assessment of your experience. If they find that you do not meet the criteria for OCD, they will still help assist you in identifying what you may be experiencing. Get Started With A Free 15 Minute Call
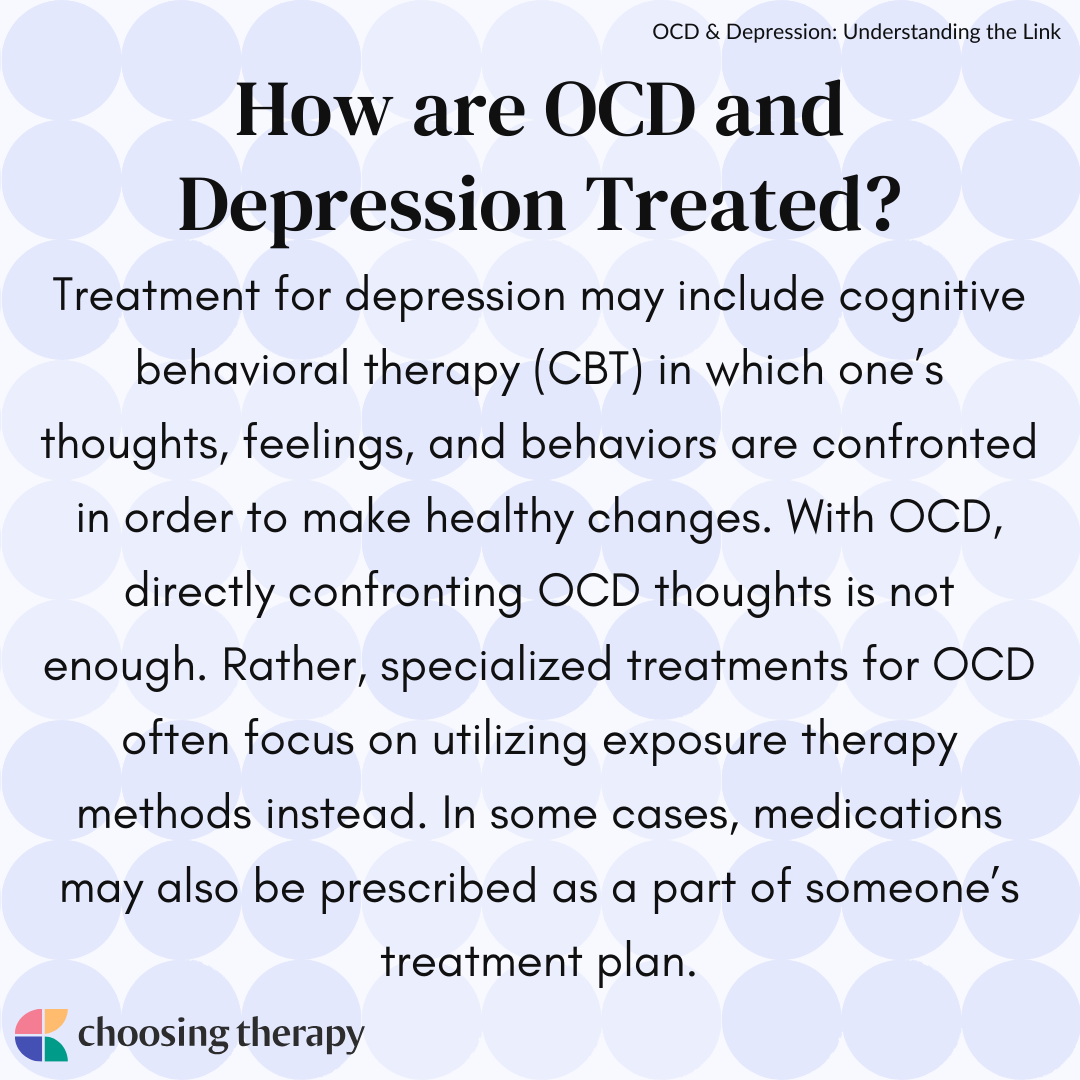
How Are OCD & Depression Treated?
Treatment for depression often involves cognitive behavioral therapy (CBT). With OCD, some components of CBT can be helpful, but directly confronting an OCD thought is not enough. Rather, specialized treatments for OCD often focus on utilizing a specific form of exposure therapy called exposure and response prevention (ERP). In some cases, medications may also be prescribed as a part of someone’s treatment plan.
Therapy for Depression
CBT for depression is usually the front line treatment, in which one’s thoughts, feelings, and behaviors are confronted in order to make healthy changes. If you are wondering whether you need therapy for your depressive symptoms, the answer is probably yes.
Therapy for OCD
An OCD therapist receives specialized training that not every provider may have. Unlike with depression, OCD requires a very specific kind of treatment that is not as generalizable. Most commonly, exposure and response prevention (ERP) is recommended in these cases. CBT includes thought-stopping techniques that may not be as beneficial for those with OCD as they are for other disorders.10 With ERP exposures, a person is slowly taught how to respond to and overcome their fears. Exposures may be “in vivo,” meaning in real life, or “imagined.”
If you think you have OCD, finding the right therapist is the first step. You should consider one who has the knowledge and skills to assess, diagnose, and treat OCD. You do not have to have a referral from a doctor to start therapy and can easily look for therapists in your area through an online therapist directory.
Medications
In addition to seeking therapy, medications may be helpful in the management of symptoms. However, medications will not simply stop obsessive thoughts and compulsive behaviors. It is important to discuss all benefits and risks of a prescription with a medical healthcare provider.
Some medications for OCD are also designed to target symptoms of depression. Seeking a consultation with a doctor will ensure that you are recommended the best options based on your personal experiences, pre-existing conditions, and genetic factors.
Deep TMS
Deep transcranial magnetic stimulation (dTMS) was FDA approved for OCD in 2018. Deep TMS is a non-invasive treatment that uses magnetic fields that activate neural networks in the brain to relieve symptoms of OCD and depression.16 During treatment, an electromagnetic coil is placed against the scalp in order to activate regions of the brain that have decreased activity in those with OCD and depression.
The research in support of dTMS is promising, showing improvement in the majority of OCD patients receiving dTMS treatment, most often within 20 treatment sessions.14 Experts suggest that dTMS may be a beneficial alternative for patients who do not respond favorably to therapy and medication, as is sometimes the case in treating OCD.15
Support Groups
For some, finding a support group to supplement individual and/or group therapy can make all the difference in finding community and peer support. Support groups typically involve a small group of people coming together regularly to offer empathy, resources, and information.They are sometimes facilitated by a therapist, but often are peer-led by a nonprofessional person. Support groups and group therapy options can be beneficial in reducing stigma and feelings of isolation, and can often be helpful as a supplement to one-on-one therapy and medication.
How to Cope If You Have OCD & Depression
Just like you would do when you have a cold or the flu, spend time finding things that help heal your mental health. Making certain lifestyle changes can improve your symptoms, such as focusing on controlling what you can. While these changes alone are not enough, they can support you throughout treatment.
Here are some tips for coping with OCD and depression:
- Seek support: Seek professional support and support from friends, family, or loved ones who you trust. Building a team of allies goes a long way, even if you choose to focus on your relationship with a therapist first.
- Practice meditation: Meditation for depression or meditation for OCD can help you build a healthier connection with your thoughts, emotions, and behaviors.
- Try journaling: Journaling can be a helpful tool to utilize when you are hesitant to share your symptoms with others.
- Determine your priorities: Determine areas of your life that need the most attention or are in urgent need of addressing. This is something that can be done with your therapist or on your own.
- List your fears: For individuals with OCD, it is important to identify, list, and arrange your fears from greatest to least worrisome. This is an important component of exposure therapy, but writing them down on your own can also be insightful.
- Be patient with yourself: As with any major life change, starting therapy and addressing your mental health can be tiring, even frustrating at times. Be patient with and forgiving of yourself as you make this journey.
- Set reminders: Remind yourself of the progress that has been made, whether this looks like starting treatment or feeling motivated to make necessary changes.
In My Experience
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below. OCD Therapy NOCD: Effective, Affordable, & Convenient OCD Therapy Do live, face-to-face video sessions with a therapist who specializes in treating OCD and get 24/7 support between sessions. NOCD is covered by many insurance plans and is available nationwide. Visit NOCD Treatment From An Online Psychiatrist Talkiatry OCD is treatable. Talkiatry specializes in OCD and provides personalized care with medication and additional support. Get started with a short assessment. OCD Newsletter A free newsletter from Choosing Therapy for those impacted by OCD. Get helpful tips and the latest information. Sign-UpAdditional Resources
What to know when finding a therapist for OCD With so much information out there regarding providers and treatment options for obsessive compulsive disorder, it can be hard to know exactly where to start—especially when you have to consider everything from the type of provider to the different treatment methods, as well as how you’ll fit it into your busy schedule. Can OCD make it hard to make decisions? From choosing what to wear in the morning to picking what to eat for dinner, decision-making is a part of everyone’s daily routine. But for millions of people with Obsessive-Compulsive Disorder (OCD), making any choice can feel like a daunting, sometimes impossible task.