Anorexia and bulimia are eating disorders characterized by preoccupations with food, weight, body image, and control. Someone with anorexia primarily relies on restricting food and avoiding eating as much as possible, while those with bulimia engage in binge/purge patterns to control their caloric intake. Both conditions can be life-threatening, and they impact people of all ages and demographics.
Struggling with your relationship with food? Do you find yourself constantly thinking about food or your body? It can be exhausting to have these thoughts. The good news is: you don’t have to feel this way. Take the first step towards healing by taking Equip’s free, confidential eating disorder screener. Learn more
Anorexia Vs. Bulimia: Key Differences
Anorexia is an eating disorder classified by disordered eating patterns, consistent food restriction, and fears of weight gain. These behaviors cause a significantly low body weight. However, the person may still perceive themselves as large, often as a result of body dysmorphia.1 Bulimia is an eating disorder classified by recurrent patterns of binging and purging. People with bulimia can be of any weight, which can sometimes make the condition harder to detect.
While most people associate purging with self-induced vomiting, purging can also include excessive exercise, laxative abuse, misusing diet pills, and diuretic abuse. Bulimia often coincides with fatigue, acid reflux, and problems with skin and hair. Eventually, bulimia can result in tooth enamel erosion, bone damage, and heart issues.
People with anorexia primarily rely on fasting and restriction to avoid gaining weight (or boost weight loss). Many with anorexia have rituals around food, avoid entire food groups, or skip meals altogether. They must be medically underweight to have a formal anorexia diagnosis (although exceptions may be made for atypical anorexia).
People with bulimia may also use these methods to control their weight, but will engage in patterns of binging and purging, too. To be diagnosed with bulimia, a person will engage in binge eating and purging at least once a week for three months. There is no specified weight criteria for bulimia.2
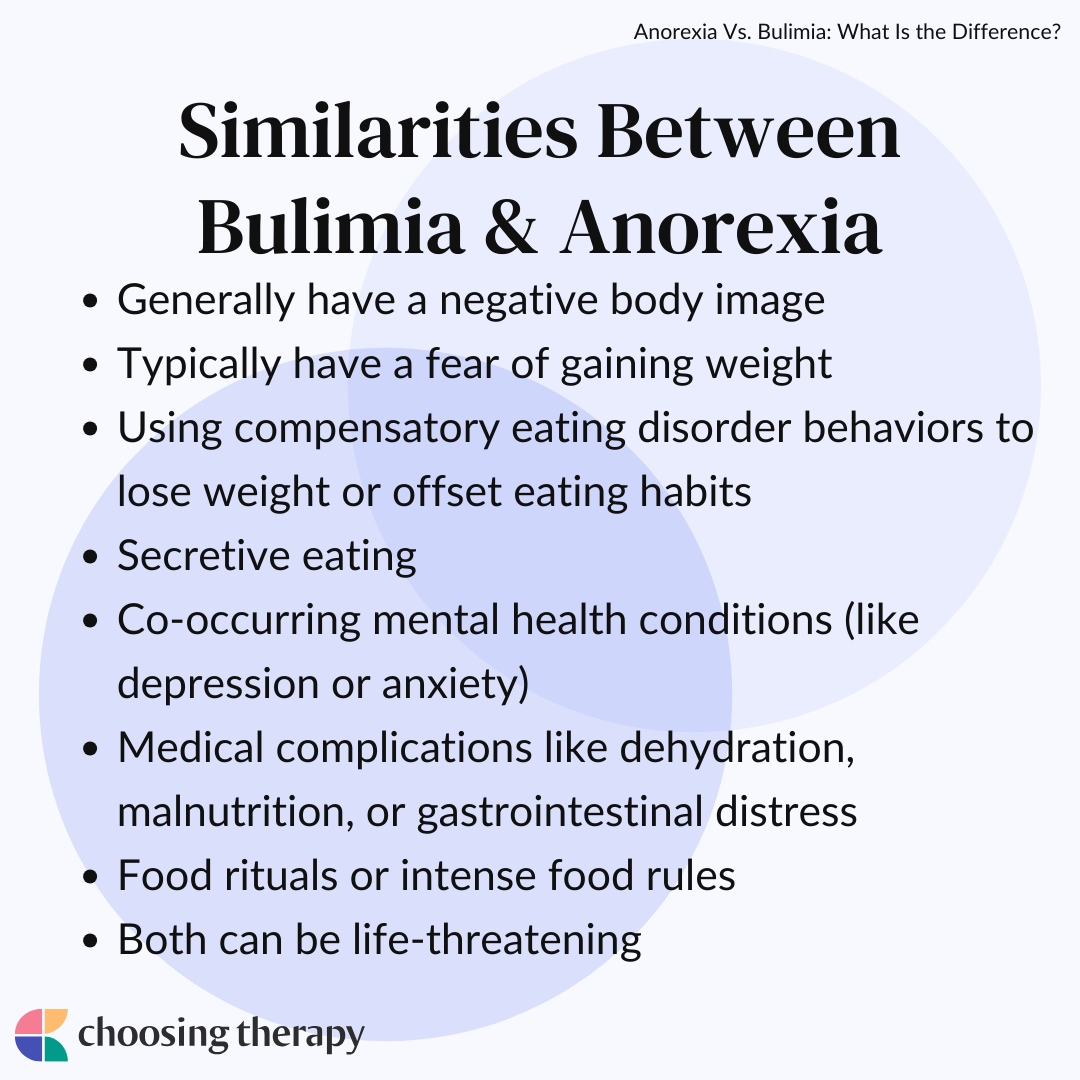
Similarities Between Bulimia & Anorexia
Bulimia and anorexia share numerous similarities. Both are eating disorders that entail a preoccupation with food and a disturbed relationship with eating. Like bulimia, some people with anorexia also engage in binging and purging. Furthermore, it’s common for people with both conditions to feel obsessed about their weight and body size.
Similarities between anorexia and bulimia include:
- Generally have a negative body image
- Typically have a fear of gaining weight
- Using compensatory eating disorder behaviors to lose weight or offset eating habits
- Secretive eating
- Co-occurring mental health conditions (i.e. depression, anxiety)
- Medical complications like dehydration, malnutrition, or gastrointestinal distress
- Food rituals or intense food rules
- Both can be life-threatening
Symptoms of Anorexia Nervosa
Anorexia impacts a person physically, emotionally, and behaviorally. At first, someone might become obsessive over food while attempting to lose weight. As a result, they may experience lethargy, poor concentration, and agitation. Over time, chronic restriction and anorexic symptoms can result in serious health consequences including malnourishment, dehydration, kidney failure, and cardiovascular problems.
Sometimes, anorexia symptoms can be obvious. But, many people attempt to hide, downplay, or deny their anorexia. They often don’t want to get into trouble, or they feel pressured to stop losing weight.
Common symptoms of anorexia include:
- Rapid and significant weight loss
- Mood swings (more agitation)
- Hair loss/dry hair
- Gray or pale skin
- Fine hair on the skin
- Avoiding meals or eating very little at mealtime
- Making frequent comments about feeling fat or wanting to lose weight
- Cutting out entire food groups
Symptoms of Bulimia
Like anorexia, people may often attempt to hide their bulimic symptoms. Loved ones should look for signs of binge eating (eating rapidly, eating secretly, or food disappearing) and purging (using the bathroom right after meals, exercising many hours a day, or evidence of laxatives or diuretics).
Common symptoms of bulimia include:
- Dehydration
- Gastrointestinal issues
- Rapid weight changes
- Dental issues
- Throat pain
- Joint or muscle injuries (from excessive exercise)
- Bowel irritation
- Skin problems
Are you or a loved one experiencing eating disorder symptoms?
A trained therapist can help! BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $65 per week. Take a Free Online Assessment and get matched with the right therapist for you.
Can Someone Be Both Bulimic & Anorexic?
Even though symptoms may overlap, people cannot meet the criteria for anorexia and bulimia at the same time. However, a person with anorexia may meet the criteria for a binge-eating/purging subtype. When this is the case, they engage in binge/purge behaviors (similar to bulimia). However, they still meet all the diagnostic criteria for anorexia (significantly low body weight, intense fear of weight gain, and disturbances with shape and size).
Anorexia is also defined by a lack of recognition regarding how serious the person’s low body weight has become.2 While many with bulimia may downplay the dangerous effects of weight loss, this is not a diagnostic feature of the condition.
What Causes Anorexia & Bulimia?
Eating disorders are caused by a variety of complex factors, and are not the result of any single variable. That said, there are several genetic and environmental factors that may increase the chance of someone developing an eating disorder.
Possible causes of anorexia and bulimia include:
- Family history of anorexia: People with first-degree relatives with anorexia are ten times more likely to have anorexia themselves. To explain this phenomenon, researchers are continuing to examine the genetic effects of serotonin, dopamine, and opioid receptors in the development of eating disorders.3
- Childhood trauma: People with eating disorders often report histories of childhood trauma.4 Controlling food and weight may be an attempt to cope with trauma-related distress.
- Sexual, verbal, or emotional abuse: Abuse can undoubtedly impact a person’s self-esteem. People may turn to focusing on their weight or food to cope with related trauma symptoms.
- Social pressures: Some people may be susceptible to societal messages about ideal appearances, thinness, and beauty. These messages may be the first trigger for disordered eating.
- Family patterns of disordered eating: Patterns of disordered eating (or obsessiveness about weight) can pass from parents to children. Children often mimic how their caregivers eat and take care of themselves.
- Anxiety and depression: Underlying anxiety or depression may drive disordered eating. Some people might self-medicate mental health symptoms with food.
- Athletic pressure: Certain sports or extracurricular activities emphasize leaner physiques or body weights. Pressure from coaches or teammates can unintentionally set a foundation for anorexia and other eating disorders.
- History of chronic dieting: Dieting may perpetuate and trigger ongoing disordered behavior, particularly in people who may be prone to anorexia.
Eating Disorder Help
Eating Disorder Treatment That Works – Delivered At Home. Eating disorder treatment is hard – which is why you deserve a team. Equip offers evidence-based care delivered virtually by a five-person care team, so you can achieve recovery without pressing pause on your life. We take insurance! Get a Consultation
Best In-Patient Treatment For Eating Disorders – Find the best local eating disorder treatment center for you. See personalized results and reviews to find the best treatment center covered by your insurance. Start Your Search
Affordable, Online Therapy – Are you or a loved one experiencing eating disorder symptoms? Get help from a licensed therapist. Betterhelp offers online therapy starting at $65 per week. Free Assessment
Complications of Living With an Eating Disorder
Both anorexia and bulimia can be extremely harmful, with severe cases often coinciding with substantial health issues. Unfortunately, these issues may be permanent if left untreated. It’s also estimated that 3.3 million people die each year from eating disorders.5 That said, the right treatment can prevent and reverse some of these complications.
Complications of Anorexia Nervosa
Complications of anorexia may include:
- Anemia
- Bone loss
- Hypertension
- Stomach ulcers
- Irregular heartbeat
- Disrupted or loss of menstrual cycle
- Peripheral neuropathy
- Organ failure
Complications of Bulimia Nervosa
Complications of bulimia may include:
- Enamel erosion
- Gum disease
- Bone damage
- Coronary heart disease
- Bowel obstruction and perforation
- Esophageal cancer
- Kidney damage
- Severe electrolyte imbalances
How Are Anorexia & Bulimia Diagnosed?
A healthcare provider will diagnose anorexia or bulimia with a variety of assessments. A doctor may perform a physical exam to evaluate someone’s pulse, blood pressure, and other vital signs. They might order lab tests to review liver, kidney, and thyroid functioning. A psychiatrist or therapist will evaluate the person’s eating habits and thoughts about food and body weight. They will refer to the DSM-5 to make an official diagnosis.
Diagnostic Criteria for Anorexia Nervosa
According to current diagnostic criteria, a person with anorexia will:
- Experience intense fears about gaining weight
- Severely restrict caloric intake to maintain or lose weight
- Connect their self-worth to their body size, weight, or food intake
- Present as underweight relative to their size or age
Diagnostic Criteria for Bulimia Nervosa
According to current diagnostic criteria, a person with bulimia will:
- Experience recurrent binge-eating episodes
- Engage in recurrent compensatory behaviors after binging
- Engage in patterns of binging and purging at least once a week for at least three months
- Strongly evaluate their worth based on body shape or weight (often presenting with very poor body image)
Eating Disorder Online Support Group Take back control with Relay, the premium binge eating program. Anonymous, flex to your schedule, all in your phone: the tool you need to finally stop binging. Try it free for a week, then subscriptions start at $9.99/month. Learn More.
How Are Anorexia & Bulimia Treated?
Many people establish recovery from anorexia or bulimia by seeking professional treatment. Treatment tends to be multidisciplinary, and people may benefit from a combination of therapy, medication, nutritional support, and positive lifestyle changes. Moreover, there are numerous evidence-based therapy models for eating disorders.
A person with an eating disorder frequently meets the criteria for other mental health conditions, including depression, substance use disorder, and anxiety. It’s important to seek comprehensive therapy or medication to treat these conditions, as well. Treating one issue without addressing the other may increase the risk of relapse.
Therapy for Anorexia & Bulimia
Finding the right therapist is often the first step in recovery. Therapy will teach you the insight and tools needed to manage your symptoms and heal from disordered eating behaviors. It’s best to look for a therapist specializing in eating disorders. Ask about their credentials, qualifications, and experience with treatment. You can start your search with an online therapist directory.
Therapy options for anorexia and bulimia include:
- CBT-E: CBT-E is a specific therapy that blends psychoeducation along with structured treatment, directly focusing on specific eating behaviors.
- Exposure therapy: Exposure therapy is a type of CBT that can help you feel more comfortable confronting fearful situations, like eating. Over time, you will experience less worry over food triggers.
- Group therapy: Eating disorder group therapy topics may include self-esteem, body image, nutrition, and healthy living. Having peer support can help you feel more validated in your recovery.
- Family therapy: Family therapy options like the Maudsley Method can provide comprehensive support for the entire family. Each attendee will be held accountable for their own thoughts and actions relating to the member with the eating disorder.
- Interpersonal therapy: In interpersonal therapy, clients focus on addressing any interpersonal conflict. In doing so, they can strengthen their confidence and self-esteem, and reduce eating disorder symptoms.
- DBT: DBT for eating disorders includes interventions rooted in mindfulness, interpersonal effectiveness, emotional regulation, and distress tolerance. These skills can improve daily coping and reduce eating disorder behaviors.
- ACT: ACT focuses on identifying and accepting the complete spectrum of emotions and thoughts. This type of mindfulness can help people manage their urges and commit toward living a value-oriented life.
- CRT: CRT aims to strengthen cognitive flexibility, which can help improve executive functioning and working memory. This approach may be beneficial for people specifically experiencing anorexia.
Hospitalization & Residential Clinics
Sometimes eating disorder symptoms can spiral into medical emergencies. If this is the case, hospitalization for the eating disorder may be necessary. Hospitalization provides continuous monitoring and evaluation; this process may also include intravenous fluids and tube feeding. Ideally, hospitalization stabilizes the most acute symptoms to provide a safe path for recovery.6
Inpatient/residential treatment (also known as rehab) may follow a hospitalization stay. This treatment also offers 24/7 support and monitoring. Length of programs vary, but they commonly last at least one month. After completing treatment, it’s important to stay active in recovery. Most clients will continue to work with a therapist and dietician.
Medication
Medication may also be an important part of one’s recovery treatment plan. The FDA has not approved any medications specifically for anorexia, but some evidence shows the benefits of antidepressants for helping reduce the risk of relapse. Research indicates the antidepressant fluoxetine (Prozac) and the anticonvulsant drug, Topamax, may reduce binge frequency for those with bulimia and binge eating disorder. Additionally, healthcare providers may recommend pharmacological treatment for other presenting mental health issues, including medications for anxiety, OCD, and mood disorders.7
Do you have a dietitian on your eating disorder recovery team? Nourish dietitians have experience with Binge Eating, Anorexia, Bulimia, and AFRID. Covered by insurance. 94% of Nourish patients pay $0 out of pocket. Visit Nourish
Recovering From an Eating Disorder
In most cases, recovering from an eating disorder can be a lengthy and complicated process. The longer someone has had an eating disorder, the longer their treatment will typically take. Recovery tends to be a multifaceted process that includes talk therapy, support groups, psychiatric medication, nutritional counseling, and family-based support.
It’s important to remember that recovery is not a linear process. People often experience setbacks throughout their journey. Relapse does not mean that someone has failed—it simply means they are experimenting with different interventions and strategies and trying to discover what works best. That said, it’s important to maintain a positive mindset throughout this time.
How to Help a Loved One With an Eating Disorder
Loving someone with an eating disorder may feel frightening, confusing, and frustrating. However, you’re not alone in your struggles. These conditions can be challenging to comprehend. But, even if you don’t understand everything, you can still help a loved one with an eating disorder. Ideally, you want to be supportive and compassionate, without assuming you know how they’re feeling.
Here are some ways to help a loved one with an eating disorder:
- Be patient: Recovery can be a long process, so you shouldn’t expect massive changes to occur overnight.
- Offer support: Let your loved one know you are there for them, and avoid making judgments when they tell you about their feelings.
- Understand the warning signs of relapse: Ask your loved one’s treatment team how you can monitor for relapse and help intervene if needed.
- Join a support group for loved ones: Many treatment facilities and therapists offer support groups for family members. These groups can help you feel validated and grounded in challenging times.
- Keep taking care of yourself: Try not to lose yourself in your loved one’s treatment or condition. It’s still important to practice self-care and maintain your own well-being, too.
- Set boundaries: Don’t enable problematic behavior. Consider seeking therapy to establish and set reasonable boundaries with your loved one.
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
Eating Disorder Treatment
Eating Disorder Treatment That Works – Delivered At Home. Eating disorder treatment is hard – which is why you deserve a team. Equip offers evidence-based care delivered virtually by a five-person care team, so you can achieve recovery without pressing pause on your life. We take insurance! Get a Consultation
In-Patient Treatment For Eating Disorders
Find the best local eating disorder treatment center for you. See personalized results and reviews to find the best treatment center covered by your insurance. Start Your Search
Online Talk Therapy
Are you or a loved one experiencing eating disorder symptoms? Get help from a licensed therapist. Betterhelp offers online therapy starting at $65 per week. Free Assessment
Eating Disorders & OCD
Is your eating disorder being made worse by OCD? Almost half of people with eating disorders also have OCD. Intrusive thoughts, including constantly thinking about food or your body, may be a sign of OCD. NOCD Therapists specialize in treating OCD and have an understanding of eating disorders. To learn more about receiving an OCD diagnosis and treatment options, schedule a free 15 minute call. NOCD is covered by many insurance plans. Visit NOCD
In My Experience
Frequently Asked Questions
Is bulimia or anorexia more common?


Research shows that bulimia is more common than anorexia. Approximately 2-3% of people have bulimia at some point in their lifetime, whereas about 0.5% have anorexia.8 Eating disorders are more prevalent in women, but men account for about 10% of all eating disorder diagnoses. That said, both bulimia and anorexia are less common than binge eating disorder and other specified feeding or eating disorders (OSFED).
When is the typical age of onset for bulimia vs anorexia?


The average age of onset for anorexia peaks at 14 and then again at 18 years of age. The prevalence of bulimia tends to be slightly later (later adolescence to early adulthood). However, in recent years, there have been younger onsets for both conditions, with some eating disorders being diagnosed as early as elementary school.9
Best Online Therapy Services There are a number of factors to consider when trying to determine which online therapy platform is going to be the best fit for you. It’s important to be mindful of what each platform costs, the services they provide you with, their providers’ training and level of expertise, and several other important criteria.

Eating Disorders: Types, Treatments & How To Get Help
If you or a loved one are dealing with an eating disorder, know you’re not alone. Treatment can significantly help improve thought patterns and symptoms that can contribute to eating disorders, and having a robust care team can be an effective prevention strategy long-term.
Find a therapist for eating disorders
Get the help you need from a therapist near you
City or zip Search