Autism and eating disorders often overlap. Autistic people commonly exhibit atypical eating behaviors, and this pattern is especially pronounced in childhood. Research shows that anywhere from 20-35% of women with anorexia meet the criteria for autism. Similarly, there is a high comorbidity between autism and avoidant/restrictive food intake disorder (ARFID).1
Struggling with your relationship with food? Do you find yourself constantly thinking about food or your body? It can be exhausting to have these thoughts. The good news is: you don’t have to feel this way. Take the first step towards healing by taking Equip’s free, confidential eating disorder screener. Learn more
What Is Autism?
Autism is a neurotype in which the ways that someone thinks, processes, and relates to the world are different from neurotypical people. Behavioral symptoms often emerge when a child is around 1-2 years old. However, most children are not diagnosed until after age 3.2 Common autistic characteristics include language delays, avoidance of make-believe play, lack of social interactions, repetitive stimming behaviors, and difficulties with transitions. However, it’s important to note that symptoms and characteristics exist on a wide spectrum.
Research shows that about 1 in 44 children has autism. It’s diagnosed four times more frequently in boys than girls.3 While once perceived as a disability, there is an ongoing conversation about destigmatizing autistic behaviors and acknowledging neurodiversity. From this framework, an autistic person simply operates differently from a neurotypical person.
What Are Eating Disorders?
Eating disorders are mental health conditions characterized by issues with food, weight gain, exercise, and control. While eating disorder symptoms vary based on the type of eating disorder and its intensity, people with eating disorders generally fixate on how, when, and what they eat. They often struggle with poor body image and low self-esteem and have a marked fear of gaining weight.
Research shows that approximately 9% of the U.S population will have an eating disorder in their lifetime. And while many people assume people with eating disorders are underweight, fewer than 6% actually are. Next to opioid overdose, eating disorders are considered the most deadly mental illness, contributing to one death every 52 minutes.4
5 Connections Between Autism & Eating Disorders
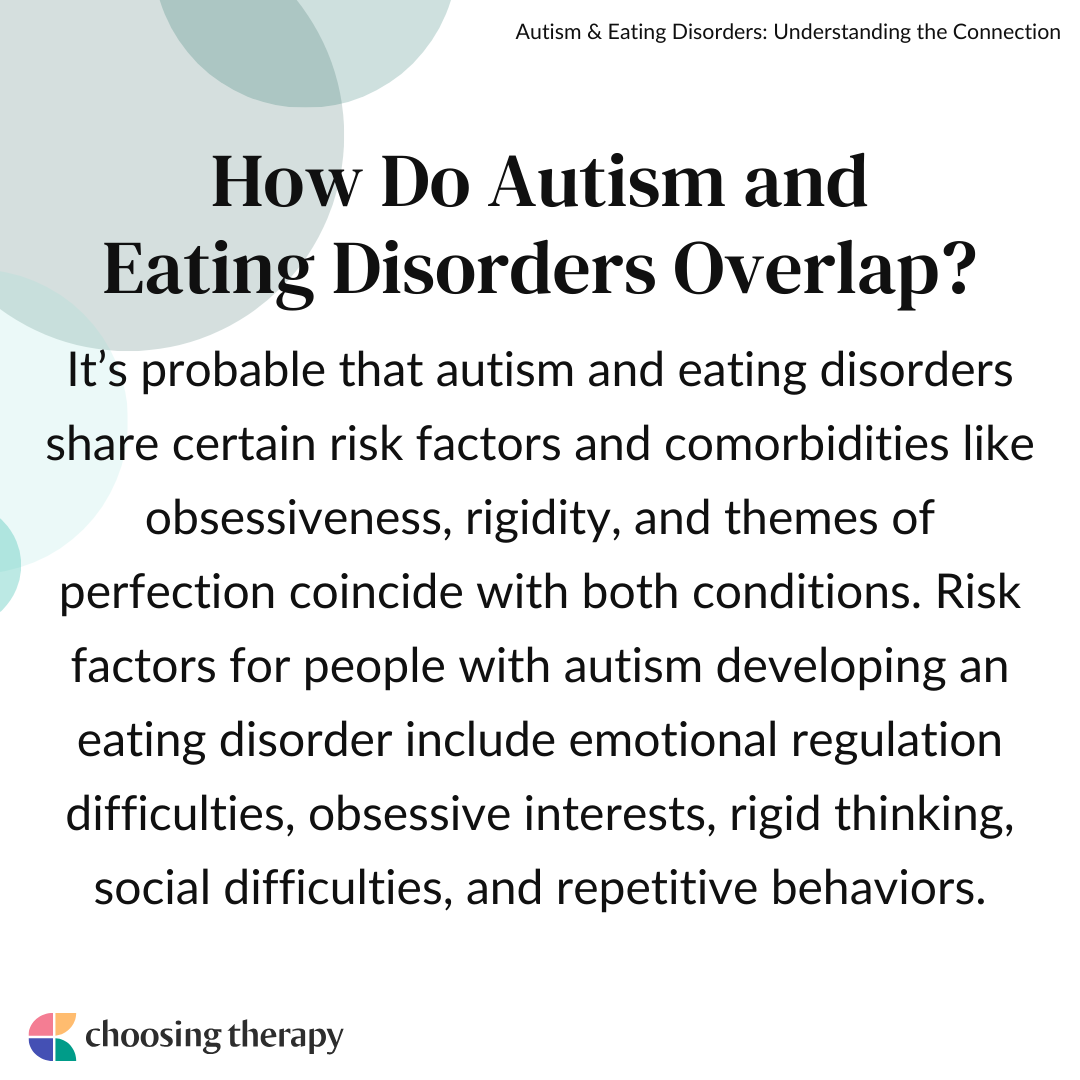
Although research isn’t sure exactly why autism and eating disorders overlap, there appears to be a strong correlation between both conditions. It’s probable that they share certain risk factors and comorbidities. For instance, obsessiveness, rigidity, and themes of perfection coincide with both conditions.5
Here are five commonalities between autism and eating disorders:
1. Emotional Regulation Difficulties
Struggles with emotional regulation are a common symptom in both eating disorders and autism. Problems with emotional dysregulation can exacerbate stress, and people may turn to restricting food or emotional eating to cope.
2. Obsessive Interests
Autism and eating disorders both entail repetitive tasks like counting calories, tracking steps, or avoiding certain types of food, which can become ritualistic. In a sense, a person with either condition may use these behaviors as a way to cope with stress and maintain a sense of control.
3. Rigid Thinking
All-or-nothing thinking is a classic symptom of both autism and eating disorders. Those with either or both diagnoses perceive certain foods or situations as ‘safe’ or ‘unsafe.’ Something is ‘good’ or ‘bad.’ The body is either ‘perfect’ or a ‘failure.’ This rigid thinking is often a result of executive dysfunction.
4. Social Difficulties
Eating disorders and autism can both include relationship problems and poor connectivity to others. Autistic people often report difficulties with intimacy and forming friendships. Subsequently, people with eating disorders often struggle with fitting in or worrying about others judging them.
5. Repetitive Behaviors
Both autism and eating disorders entail ongoing, repetitive behaviors that cause significant distress when interfered with. Someone with anorexia may count calories due to poor body image and a desire to lose weight. Similarly, an autistic person may ritualistically count calories or compulsively exercise, even if weight loss isn’t the intended goal.6
Do you have a dietitian on your eating disorder recovery team? Nourish dietitians have experience with Binge Eating, Anorexia, Bulimia, and AFRID. Covered by insurance. 94% of Nourish patients pay $0 out of pocket. Visit Nourish
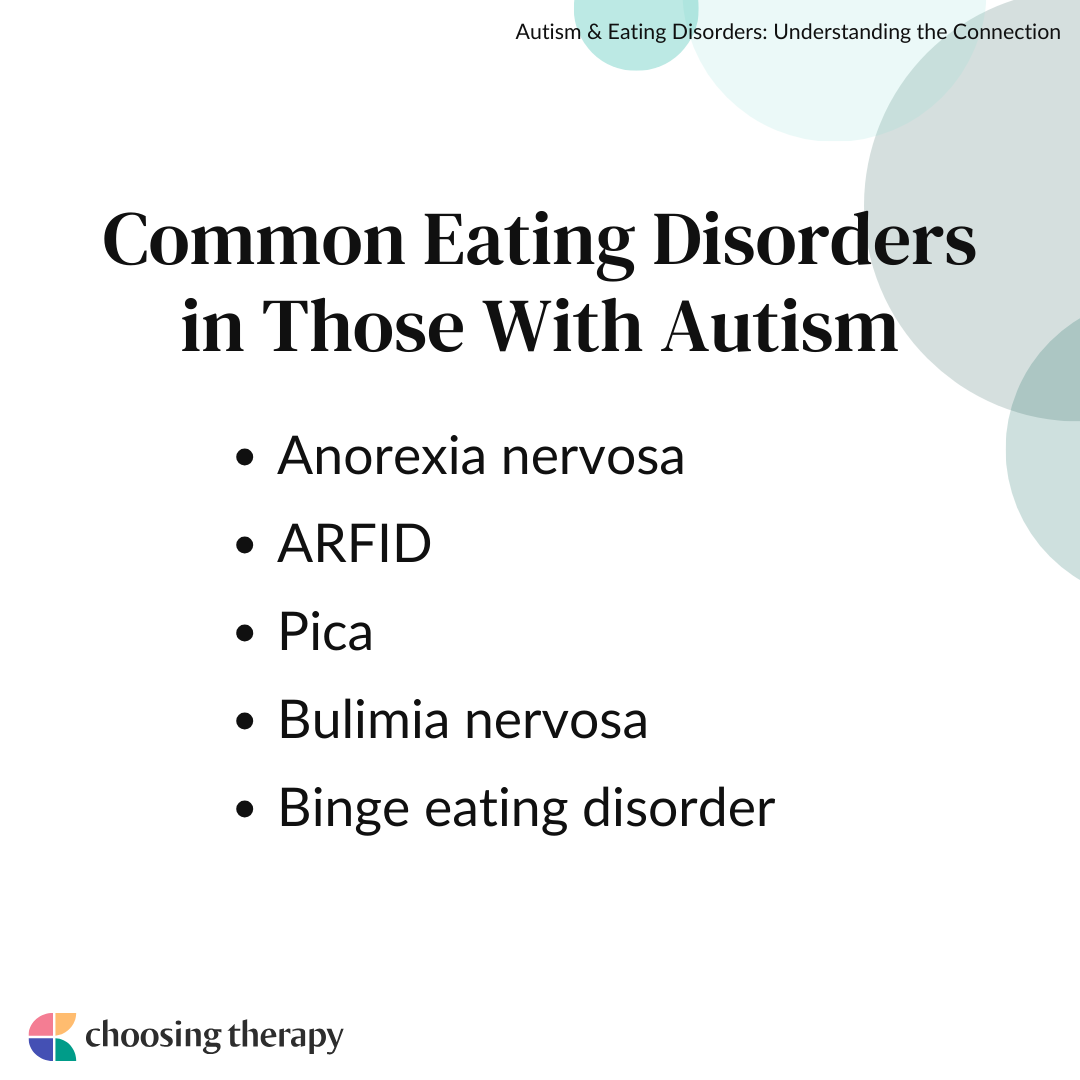
Common Eating Disorders in Autism
Autism can correlate with any eating disorder, but comorbidity appears to be highest with anorexia and ARFID. For instance, although only 1% of the population is autistic, and 0.3% have anorexia, 20-35% of people with anorexia are autistic.1 Some research suggests that those with autism are five times more likely to be diagnosed with anorexia than non-autistic people.6 Furthermore, statistics on co-occurring autism and ARFID are around 33%.7 Children and young adults appear to have the highest rates of comorbidities.
It’s important to keep in mind that these studies and statistics are likely misrepresented. Most eating disorder research focuses on girls and women, and most autism research focuses on boys and men. Therefore, there may be some inconsistencies and missing data.
Autism & Anorexia Nervosa
Anorexia nervosa is an eating disorder characterized by chronic and consistent food restriction and a preoccupation with body image. People with anorexia are hyper focused on avoiding weight gain. However, the eating disorder symptoms often represent themes of control, perfectionism, and fear. Anorexia may be a coping mechanism to avoid stress or interpersonal difficulties. These symptoms often overlap with autistic symptoms of rigidity, control, and a preference for having a strict routine.
Autism & ARFID
ARFID refers to having little to no interest in eating food. People with ARFID aren’t worried about their weight or body size, but they do experience disgust and apathy towards eating. This overlaps with autism, as autistic people often experience sensory issues and difficulties with certain food textures, smells, or tastes. This is particularly pervasive among children, and it can cause ongoing food battles.
Autism & Pica
Pica is an eating disorder characterized by compulsively consuming non-food items (such as clay, dirt, paint, or glue) that have no nutritional value. Research shows that one in four parents report their young autistic child ‘sometimes’ eats non-food items.8 This pattern likely stems from limited food preferences, sensory processing difficulties, and intellectual disabilities that make it challenging to distinguish edible food from non-food items.
Autism & Bulimia Nervosa
Bulimia refers to patterns of binge eating (eating large amounts of food rapidly) and purging (self-induced vomiting, excessive exercise, abusing diuretics or laxatives). A person with bulimia can be rigid in their thinking (i.e., having safe and unsafe foods), although they also experience the perception of “losing control.” These patterns may also be present in autism, as autistic people often experience significant distress when a situation feels out of their control.
Autism & Binge Eating Disorder
Binge eating disorder is an eating disorder characterized by routinely bingeing without taking compensatory measures. People with this condition often use food as a way to cope with stress or numb their feelings. Some research has shown that autistic people can sometimes exhibit overeating tendencies in childhood. This pattern may be due to hypersensitivity and pleasure to certain textures.9
Resources For Autism
Sensory Enrichment Program For Autism – Boost brain development to give your child more tools. Top 5 areas of improvement reported are Attention, Sleep, Sensory Processing, Eating, and Social Skills. Learn More
Pediatric Mental Healthcare For Autism Spectrum Disorder (ages 1 -17) Bend Health does not provide ABA Therapy. Bend Health is a virtual-first mental health care provider caring for kids, teens and their families. Build skills and routines that support your whole family with coaches, therapists and psychiatrists. For parent’s, Bend offers monthly progress updates and a peer support community. Many insurance plans are accepted. Learn More
Neuropsychological Testing For Children (including evaluations for Autism Spectrum Disorder, ADHD and Learning Disorders) Get answers in weeks, not months. Bend Health provides a complete report with in-depth findings, review with your schools, and a clinical diagnosis (if applicable). Learn more
Eating Disorders Vs. Picky Eating
Autism and picky eating often go hand-in-hand. But, being picky is not inherently synonymous with disordered eating. Someone who is picky may have strong preferences about what they like (and don’t like) to eat. However, their food choices aren’t directly related to body image or weight control.
A picky eater may unintentionally restrict because they feel uncomfortable eating specific foods. In serious cases, young children go through entire periods of food refusal. But the restriction isn’t about controlling intake. Picky eating is also a common symptom of sensory processing disorder (SPD), a condition associated with being very particular about certain textures, smells, or tastes.
Are the Causes of Autism and Eating Disorders Connected?
Mental illness is multifaceted, and there are no definite causations for either autism or eating disorders. Instead, a complex constellation of variables may increase someone’s chance of developing one (or both) of these conditions.
Possible causes for autism and eating disorders include:
- Genetics: Specific gene combinations may affect brain development and impact how cells communicate, determining the severity of specific symptoms. We are likely in the early infancy stages of this neuroscience, and researchers are still examining these relationships.
- Family history: Families with one child with autism or an eating disorder have an increased risk of another child having those disorders. Similarly, there are links between parents having these conditions and their children having them.
- Preterm birth: Some research shows that babies born prematurely (before 32 weeks gestation) have a greater risk of developing autism and anorexia.10,11
- Advanced paternal age: Although there hasn’t been extensive research on this topic, some data suggests that older paternal age is associated with an increased risk for various mental health disorders, including autism and eating disorders.12
- Environmental factors: Researchers are examining the relationship between autism, eating disorders, and different environmental risk factors, including low birth weights, prenatal exposure to pollution and pesticides, and early birth difficulties.
How Are Co-Occurring Eating Disorders & Autism Treated?
Comprehensive treatment needs to consider both the distinction and overlap of the eating disorder and any relevant autistic symptoms. Effective treatment should be multifaceted, and a thorough mental health assessment is essential. For instance, many people with eating disorders may have undiagnosed autism, and vice versa.
If you’re ready to get treatment, consider asking your primary care physician for a referral, using an online therapist directory where you can sort by specialty and insurance coverage, or using an online eating disorder treatment platform like Within Health or Equip Health.
Options for treating eating disorders in people with autism include:
- Play therapy: Play therapy provides interactive support, and it can be especially helpful for younger clients. It can help people understand their thoughts and feelings without direct talk therapy.
- Cognitive-behavioral therapy (CBT): CBT offers guidance in modifying negative or unhelpful thinking patterns, and replacing them with healthier ones. It also introduces adaptive coping skills for coping with triggering situations.
- Enhanced cognitive-behavioral therapy (CBT-E): CBT-E is specifically designed for eating disorders. It blends concepts of psychoeducation, cognitive restructuring, and changing problematic eating disorder symptoms.
- Acceptance and commitment therapy (ACT): ACT blends mindfulness and behavioral interventions. This therapy ultimately helps people identify their values and live congruently with them.
- Family therapy: Family therapy can empower people to provide support to their loved ones with an eating disorder and autism. This therapy also teaches healthy communication and reinforces boundaries and safety.
Neuropsychological Testing For Children Get answers in weeks, not months. Bend Health provides a complete neuropsychological report with in-depth findings, reviews with your school or pediatrician, along with a clinical diagnosis (if applicable). Plus, receive recommendations to support your child at home, in the community, and in the classroom. Learn more
How to Cope With Autism & Eating Disorders
At times, having comorbid autism and an eating disorder may feel challenging. Depending on the severity of your symptoms, it might also seem like things will never get better. Implementing healthy lifestyle habits and considering professional treatment can make a significant difference in improving how you feel.
Here are some ways to cope with an eating disorder when you’re also autistic:
- Build a healthy peer support system: It’s important to have reliable friends and family who can validate you. If talking to people feels overwhelming, consider finding an online group or forum.
- Keep your hands occupied: Sensory and fidget toys can help with the restlessness that coincides with both disorders. These objects can also encourage mindfulness.
- Practice positive affirmations: Remind yourself that you can cope with challenging circumstances and learn from your hardships.
- Stick to a routine: Autistic people tend to thrive with routine. Aim to build a healthy routine that balances self-care with your typical responsibilities.
- Change your environment: If you feel stressed in a particular setting, consider leaving altogether. Before you attend an event that may feel triggering, consider brainstorming an exit strategy.
- Hold onto grounding items: Designate a small rock, coin, or other tangible item that promotes a sense of calm. The next time you feel triggered or overwhelmed, hold onto that item as a reminder that you can get through this moment.
- Take a few deep breaths: Close your eyes and inhale as deeply as you can. Then, exhale as deeply as you can. Repeat at least five times.
- Find a creative outlet: Consider journaling, painting, drawing, or taking photos as part of your wellness plan.
- Celebrate small successes: Recovery from an eating disorder is rarely linear. Make it a point to acknowledge all steps taken in the right direction, no matter how small they may seem.
Neuropsychological Testing For Children Get answers in weeks, not months. Bend Health provides a complete neuropsychological report with in-depth findings, reviews with your school or pediatrician, along with a clinical diagnosis (if applicable). Plus, receive recommendations to support your child at home, in the community, and in the classroom. Learn more
In My Experience
Frequently Asked Questions
How can an eating disorder treatment team make a treatment plan that fits the unique needs of someone with autism?


It’s important for the treatment team to be aware that autism is not a one-size-fits-all condition. Every autistic person is different, and, based on their eating disorder concerns, each client will have different needs, strengths, and treatment preferences. In general, it’s key to be mindful of an autistic’s client’s potential sensory issues and their desire for structure and predictability.
How does autism affect eating?


Autism can impact habits in several ways. Autism may coincide with sensory sensitivities, which can impact eating habits. People may have heightened aversions to certain tastes, textures, or types of food. They may also have preferred eating rituals that can feel rigid or obsessive. Some autistic people also have co-occurring issues related to anxiety or depression, which can make them more prone to seeking food for comfort.
What percentage of autistic people have an eating disorder?


The exact percentage of autistic people with eating disorders is unknown. This is because both conditions are often underdiagnosed or misdiagnosed. However, some research suggests that anywhere from 4-24% of people diagnosed with eating disorders also have autism. Anorexia appears to be the most common eating disorder diagnosis, but autistic people may also experience other eating disorders.13
What challenges might someone with autism face when trying to get the right treatment for their eating disorder?


Autistic people may present as “resistant” to treatment, although this resistance is usually an expression of difficulties associated with change, flexibility, and social connection. Some autistic people struggle to open up about their emotions, which can make it difficult for them to engage in the treatment process. Similarly, they may also have co-occurring mental health issues, including PTSD, anxiety, or depression.
How to help a child with OCD and Autism If you have an autistic child, they might exhibit some behaviors that look similar to compulsions in OCD, like having to wear certain clothes, lining up toys in a certain way, or engaging in specific routines & rituals. OCD rituals, aka compulsions, can look similar to the repetitive behaviors common in Autism, as a 2011 study found that about 17% of people with an Autism Spectrum Disorder (ASD) also meet criteria for OCD.
Find a therapist for eating disorders
Get the help you need from a therapist near you
City or zip Search