Many people diagnosed with schizophrenia experience symptoms of depression, or vice versa. Sometimes these folks meet criteria for both schizophrenia and depression; other times a diagnosis that captures both groups of symptoms–like major depressive disorder with psychotic symptoms or schizoaffective disorder–could be more accurate.
Schizophrenia Treatment, Covered by Insurance Grow Therapy enables you to find a psychiatrist or psychiatric nurse practitioner who can diagnose your condition, prescribe appropriate medications, and monitor your reaction to medication. Find A Provider
What Is Schizophrenia?
People with schizophrenia tend to experience symptoms such as hallucinations, delusions, disorganized thinking, difficulties concentrating, and challenges to complete day-to-day tasks. Schizophrenia is the most commonly known psychotic disorder, and impacts about 1% of the population.
Most men with schizophrenia will have their first episode of psychosis between the ages of 18-25, while this may occur later for women. However, many people experience some mild symptoms before their first episode, in the “prodrome” stage of schizophrenia. In these cases, a person may be able to receive a proactive diagnosis through clinical assessment. Thus, treatment can help reduce their risk of having a future episode and decrease the severity of those episodes.
Symptoms of schizophrenia are often separated into five categories:
- Positive symptoms: “Positive” refers to symptoms a person experiences that others do not (they are “added”). These include hallucinations and delusions.
- Negative symptoms: “Negative” indicates typical experiences that a person with schizophrenia doesn’t have (they are “subtracted”), such as difficulty feeling or expressing emotions.
- Disorganized symptoms: These symptoms include disorganized or confused thinking, or disorganized physical behavior that gets in the way of a person’s ability to interact with others or their environment. It doesn’t refer to being disorganized in the sense of keeping a space clean.
- Excited symptoms: These symptoms are also often associated with mania, and may include an overly elevated mood, high levels of distractibility, and physical hyperactivity.
- Depressive symptoms: These symptoms include low mood, low motivation, loss of interest, and fatigue.
What Is Depression?
Depression (or “major depressive disorder”) is a very common mental illness that impacts about 8.4% of American adults and 17% of American adolescents per year.1 Depression can occur for many reasons, including loss, grief, and trauma; but, it can also occur for seemingly no reason at all. Common symptoms of depression include sadness, lack of interest or pleasure in things that used to bring joy, and fatigue that doesn’t improve with rest.
Other common symptoms of depression include:
- Feelings of worthlessness
- Feelings of guilt or shame
- Rumination, or thinking about painful things over and over
- Difficulty with sleep (sleeping too much or too little)
- Difficulty with eating (no appetite, feeling hungry even after eating, using food to cope)
- Feeling like you might want to die, or considering ending your life
Comorbid Schizophrenia & Depression
About 50% of people with schizophrenia also experience depression.2 Because depression and other mood symptoms are so common in those with schizophrenia, many experts argue that these conditions and schizophrenia co-exist on a spectrum of overlapping mental health conditions. Additionally, there are specific diagnoses that include both of these groups of symptoms, the most common of which are schizoaffective disorder and major depressive disorder with psychotic features.
The easiest way to spot the difference between these disorders comes from the primary set of symptoms being experienced. These symptoms usually occur first, are more dominant and impactful, and may lead to symptoms of the other conditions (i.e., major depressive disorder). For example, if schizophrenia symptoms are primary, then depressive symptoms most likely indicate schizoaffective disorder. Conversely, primary depressive symptoms typically suggest major depressive disorder with psychotic features.
However, sometimes there isn’t an identifiable primary set of symptoms. The symptoms of schizophrenia and depression may be independent enough from each other that a person can be diagnosed with both disorders, rather than a combined diagnosis.
Resources For Schizophrenia
Treatment for Schizophrenia, Covered by Insurance – Grow Therapy enables you to find a psychiatrist or psychiatric nurse practitioner that can diagnose your condition, prescribe appropriate medications, and monitor your reaction to medication. Find A Provider
Schizophrenia Newsletter – Free newsletter from Choosing Therapy for those impacted by Schizophrenia. Get encouragement, tips, and latest info sent twice per week. Sign Up
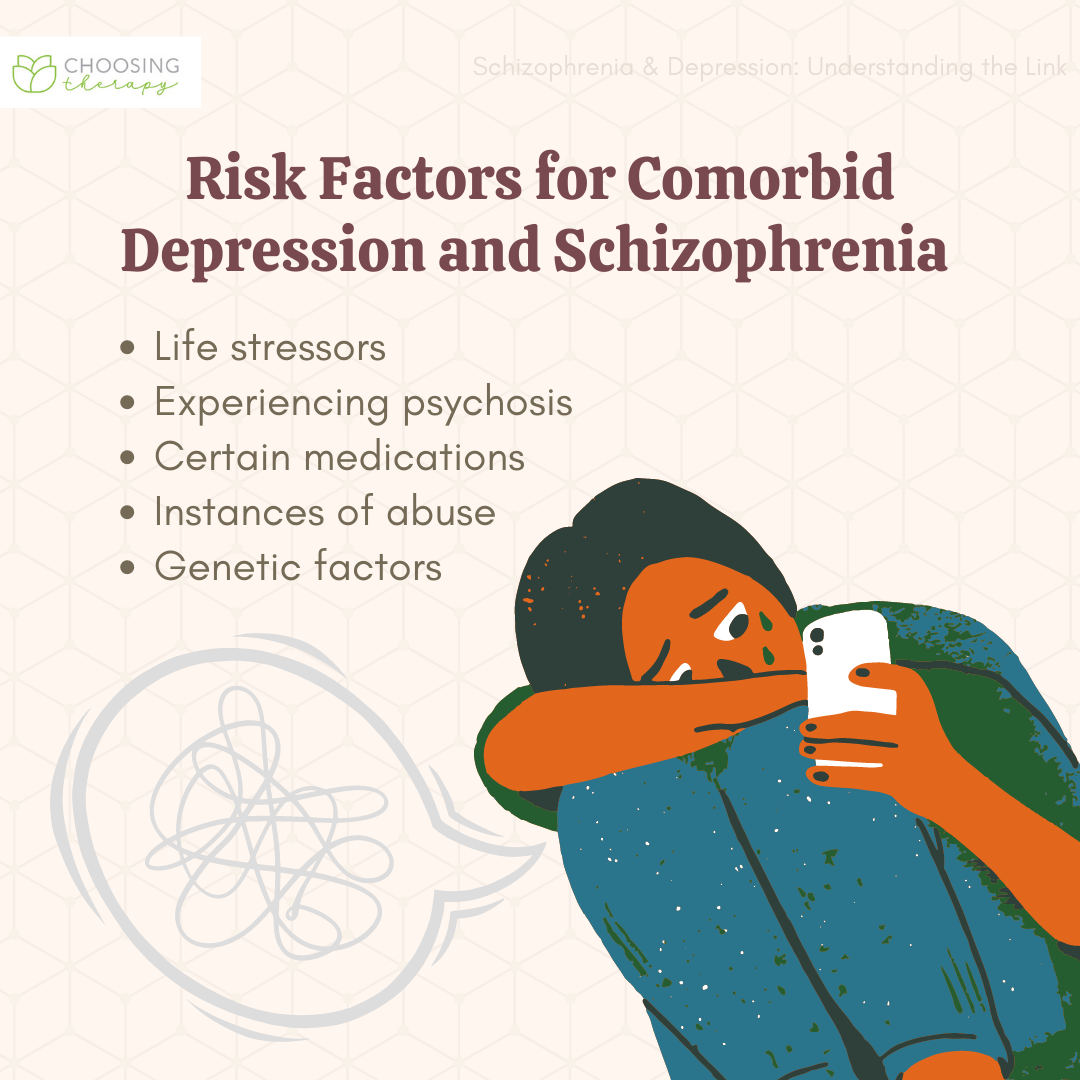
Risk Factors for Comorbid Depression & Schizophrenia
There are multiple reasons why a person with schizophrenia may also experience depression, including instances of trauma, medication side effects, among others. For instance, the experience of having schizophrenia on its own can be very difficult or traumatic. This can in turn heighten one’s risk for developing typical symptoms of depression.
Possible causes of comorbid depression and schizophrenia include:
- Life stressors: Experiencing inpatient hospitalization; having to take leave from school or work; changes in self-identity; and difficulties within personal relationships due to schizophrenia symptoms may lead to sadness, grief, guilt, and self-stigma.
- Experiencing psychosis: Specific parts of psychotic episode cycles are associated with depression symptoms, including the prodrome (meaning, before the first episode) and the postpsychotic interval (meaning, after each episode).
- Certain medications: Common medications for schizophrenia can sometimes cause symptoms of depression such as fatigue, low energy, low mood, and low motivation.
- Instances of abuse: Experiencing childhood trauma or abuse can increase the risk of developing depression symptoms in those with schizophrenia.3
- Genetic Factors: Some individual traits also appear to increase risk of experiencing depression alongside schizophrenia including having genetic risk factors for depression.3
Does Depression Make Schizophrenia Symptoms Worse?
Those diagnosed with both schizophrenia and depression tend to have more chronic symptoms and a higher rate of relapse.2 Therefore, finding the appropriate treatment is critical to better manage the challenges that accompany these conditions.
Treatment for Comorbid Schizophrenia & Depression
It can be overwhelming to experience symptoms of schizophrenia and depression. You might feel like other people won’t understand what you’re experiencing or judge you. This is absolutely understandable–stigma is a real problem. However, finding the right clinicians can make a world of difference. Experts in schizophrenia and depression may not have walked in your same shoes, but they have the training, empathy, and compassion to support you and help you effectively. Treatment for schizophrenia and depression will likely include medication, therapy, and lifestyle changes. Severe cases may require hospitalization.
A treatment plan for those with comorbid schizophrenia and depression may include:
Medications
Most commonly, a combination of medications targeting schizophrenia symptoms (usually called “antipsychotics”) and depression symptoms (usually called “antidepressants”) will be incorporated into a treatment plan. However, when taking multiple psychoactive medications, it is important to work closely with your doctor and pharmacist.
Some prescriptions, particularly antidepressants, can cause serotonin syndrome when taken together and/or in too high a dose, which can be very serious or fatal. Some medications cannot be taken with alcohol or other recreational substances. It is essential to be honest with your prescriber about the substances you use to ensure you are not ingesting combinations that will be unsafe for you.
A medication regimen for treating comorbid schizophrenia and depression may include:
- Typical antipsychotics: Also known as first generation antipsychotics, these were the first medications approved for schizophrenia and related symptoms. They tend to be most helpful for hallucinations and delusions.
- Atypical antipsychotics: Also called second generation antipsychotics, these tend to be most helpful for hallucinations and delusions.
- Antidepressants: Antidepressants aim to improve mood, motivation, and energy. Common types of antidepressants include SSRIs, SNRIs, and MAOIs.
- Injectables: Some typical and atypical antipsychotics are available via injection. Injectables provide consistent doses throughout a month or several months, and can be particularly helpful for those who have trouble remembering to take medications.
- Ketamine: Early research has found some evidence that ketamine is helpful for depression. Doses may be administered just once or for a short period under the supervision of a medical provider. However, it has not yet been tested for those with comorbid schizophrenia.
Therapy
Therapy can help a person with schizophrenia and depression target specific symptoms, improve daily functioning, or simply enhance one’s quality of life. There are benefits of therapy regardless of one’s diagnosis, as long as the option you choose aligns with what’s important to you. At the same time, research identifies specific therapies that work best for depression and for schizophrenia. These will be the most likely to help you reduce symptoms and start your healing journey.
Finding the right therapist or specialist team can be incredibly beneficial. Additionally, certain coordinated specialty care programs for those with first episode psychosis symptoms or schizophrenia may provide the support you need. Your primary care doctor, current psychiatrist, or neurologist might be able to refer one of these programs to you. To locate a therapist, you could start by using an online directory. Local and online resources like NAMI and the Hearing Voices Network, can put you in touch with others
Therapeutic options for comorbid schizophrenia and depression include:
- Cognitive behavioral therapy (CBT): CBT helps you understand the relationship between your thoughts, feelings, behaviors, and environment. CBT helps people make important changes in their beliefs and behaviors, leading to an improved self-image and mood.
- Acceptance and commitment therapy (ACT): ACT is a values-based therapy that incorporates mindfulness and other practice-based strategies to help people act in alignment with their values, and gain distance from negative thoughts. This can help improve mood and quality of life.
- Family therapy: For those with schizophrenia and depression, family therapy is often used to help provide psychoeducation to family members about mental illness, and identify helpful strategies to provide support.
- Cognitive rehabilitation: For people who are experiencing problems with memory, attention, concentration, and problem-solving, cognitive rehabilitation can help improve cognitive functioning.
- Social skills therapy: Sometimes folks with schizophrenia and depression struggle with specific or general social skills. Social skills therapy can help by providing a space to practice skills you are struggling with. It is usually facilitated with therapists and a group of participants.
- Group therapy: Group therapy can be helpful because you can talk through your experiences and receive support from like minded individuals.
Hospitalization
Sometimes those diagnosed with schizophrenia and depression are hospitalized when symptoms become unmanageable. This might be for only a few days, or for a few weeks or months. You may choose to seek hospitalization on your own volition in order to keep yourself or others safe. Alternatively, if a provider or another professional believes a person is at imminent risk of harm to themselves or others, they may be placed in a facility involuntarily.
Inpatient experiences vary quite a bit, but there are often group therapy and other activities offered. A patient might have the option to meet with a therapist individually, too. Access to medication is provided, and alternative treatments for schizophrenia, such as ECT, may also be provided. Hospitalization can be stressful, so communicating your needs and sticking to a routine can be helpful.
How to Cope With Comorbid Schizophrenia & Depression
It can be difficult to cope with schizophrenia and depression. Creating your own personalized set of healthy coping mechanisms can make life more manageable and enjoyable. Your coping plan should be personal to you, based on things you enjoy, and beneficial for your own mental health. These steps can also change over time. You might find that you’ve grown out of something you once enjoyed, and choose to replace it with another activity. You may create your coping plan on your own, but it can be helpful to receive input from people you trust, including your therapist, friends, and family.
Here are some self-coping skills to consider:
- Remember the basics: Maintaining a grooming and hygiene routine is important when coping with any condition. Integrating some things you really enjoy into that routine can help you get it done on tougher days. Try listening to a curated playlist of favorite songs while you shower, or using a really delicious smelling lotion. Remember that something is better than nothing, so consider having a shorter routine ready for days you’re unable to get the whole thing done.
- Integrate values into daily life: Try a values sort exercise if you would like to identify values that are important to you. Your coping plan should include activities that align with your beliefs and needs. For example, if art is important to you, your coping plan might include drawing, writing, or painting a couple times a week.
- Social connection: Connecting to other people is important. This might include family, friends, partners, social groups, or online communities. Structured activities, including volunteer work, can be a good way to spend time around others in a productive way.
- Self-soothe: Self-soothing is a way to reduce stress in tough moments. By tapping into one or more of your five senses with something you find comforting, you can activate your parasympathetic nervous system and calm your anxiety.
- Practice emotional self-care: Emotional self-care often includes things that are hard at first but have big impacts on your wellness long-term. For example, this may include setting healthy boundaries with other people.
- Gratitude practice: People have a natural tendency to remember the bad more than the good. Actively engaging in “pleasure savoring” and extending gratitude can help us remember the positive parts of life. You can do this by journaling or writing gratitude letters to people who have made an impact on you (whether you send them or not). There are any number of ways to practice gratitude, so don’t limit yourself!
- Journaling: Journaling for one’s mental health can look differently for everyone, depending on their needs. You can write a lot or a little–it’s up to you. Journaling helps many people organize their thoughts, identify helpful and unhelpful patterns of thinking, and provides a creative outlet when you need it.
Final Thoughts
About half of people with schizophrenia also experience depression. If this is you, know that you are not alone in your struggles. It’s often hard to deal with both sets of symptoms at once, but treatment is available. There are also numerous other helpful resources from which you can benefit.
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
Treatment for Schizophrenia, Covered by Insurance – Grow Therapy enables you to find a psychiatrist or psychiatric nurse practitioner that can diagnose your condition, prescribe appropriate medications, and monitor your reaction to medication. Find A Provider
Talk Therapy – BetterHelp has 25,000+ licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $65 per week. Visit BetterHelp
Schizophrenia Newsletter – Free newsletter from Choosing Therapy for those impacted by Schizophrenia. Get encouragement, tips, and latest info sent twice per week. Sign Up
For Further Reading
- Hearing Voices Network
- NAMI
- Akin Mental Health (for loved ones of people with mental illness)
- Students with Psychosis
- SAMHSA’s Living Well with Schizophrenia
- SAMHSA’s Early Serious Mental Illness Treatment Locator (to help you find treatment if you are experiencing your first episode of schizophrenia or psychosis)
- Value Card Sort
- 21 Books on Depression
- 15 Best CBT Apps
Fears about schizophrenia – What do they mean? If you’re experiencing unwanted thoughts about losing your mind, becoming psychotic, or developing schizophrenia, it may actually be a sign of OCD more specifically health concern OCD. You might find yourself constantly questioning the state of your mind, which can cause you to be overly focused on feeling different than usual.