Postpartum obsessive-compulsive disorder (OCD) is a perinatal disorder that can develop after someone gives birth. People with this condition experience obsessive thoughts that are difficult to control, and engage in compulsive behaviors to help relieve the anxiety caused by the obsessions. While postpartum OCD can be distressing for new parents, it is treatable with medication, therapy, and self-care.
What is the best therapy for Postpartum OCD?
Exposure And Response Prevention Therapy (ERP) – Do live video sessions with a therapist specialized in ERP, the gold standard treatment for OCD. Treatment from NOCD is covered by many insurance plans. Start With A Free 15 Minute Call
What Is Postpartum OCD?
Obsessive compulsive disorder (OCD) involves intrusive, hard-to-control thoughts that are distressing.1 People may try to ignore the obsessions or engage in certain acts or rituals called compulsions to help cope. Around half of people experience intrusive thoughts postpartum, however, only a portion of these symptoms are severe enough to be considered OCD.
The most common postpartum OCD obsessions are about germs, contamination, and harm coming to the baby, either accidentally or on purpose.2 For example, someone may have thoughts about dropping the baby or fear that the baby could stop breathing. In response, they may repeatedly clean, check, avoid certain places or situations, and/or try to suppress those thoughts. A key feature of postpartum OCD is that people find their obsessions to be upsetting and scary.
OCD tends to develop in response to stress.2 Giving birth and becoming a parent is a stressful experience, which explains why new parents are at increased risk of developing OCD. Certain people may be at higher risk of developing OCD after giving birth, especially those with a history of OCD or other anxiety disorders.3
How Common Is Postpartum OCD?
OCD occurs during or post pregnancy in about 4-9% of cases, which is higher than the average rate of OCD at 1.2% of the general population.4,5 Some experts believe rates may be higher, but people may be unlikely to seek help due to shame and mental health stigma.5 Additionally, some professionals may not have received training on perinatal or postpartum OCD as a specific subtypes and misdiagnose the symptoms as perinatal or postpartum depression.4
Rates of diagnosis tend to be higher among people who had an OCD diagnosis prior to pregnancy.6 Most cases of postpartum OCD peak around 8 weeks after childbirth and steadily decline after this point.5
Can Men Have Postpartum OCD?
Postpartum OCD can occur in all parents, regardless of whether or not they are a birth parent.7 Since Postpartum OCD happens due to a combination of hormonal, medical, and environmental factors, it can happen in fathers even though they do not give birth.7 Experts believe that adjusting to parenthood, as well as the effects of hormones associated with childbirth, sleeplessness, and responsibility following the birth of a child may play a role in developing postpartum OCD, meaning that parents can be diagnosed regardless of their identified gender.7
How Is Perinatal OCD Different From OCD That Occurs at Other Times?
Perinatal OCD and OCD that develops at other points in a person’s lifetime share the same symptoms, including the presence of obsessive thoughts and/or compulsive behaviors.8 The main difference is when symptoms begin. For someone to be diagnosed with postpartum OCD, the symptoms must develop or worsen during the postpartum period (any point within a year after giving birth).
One difference that has been found between postpartum OCD and OCD that occurs at other times is that people with postpartum OCD are more likely to have obsessions about harm coming to their babies. This can include obsessive thoughts or images of dropping or poisoning the baby. People with postpartum OCD may also experience other types of obsessions, such as those involving cleanliness, order, or religion.
How Long Does Postpartum OCD Last?
Postpartum OCD typically develops within two to four weeks of giving birth.3 There is no specific timeline for how long postpartum OCD may last. For some people, symptoms begin shortly after giving birth. Other women may experience OCD during pregnancy or before getting pregnant, but find that their symptoms become worse after delivery. Postpartum OCD may not go away on its own. Treatment, including therapy and medication, may be needed to recover from this condition.
Normal New Mother Fears Vs. OCD
While most new parents worry about their baby’s health and well-being, if thoughts become intrusive, unwanted and disturbing, or impact their ability to function, they may be experiencing symptoms of OCD.
Obsessive thoughts in those with postpartum OCD might be related to fears of:6
- Accidentally harming the baby
- Someone else harming the baby
- The baby getting sick or dying
- Putting the baby down somewhere dangerous or
- Forgetting about the baby
Related compulsions might include:6
- Excessively checking on the baby
- Not allowing another adult to hold or care for the baby
- Requiring another adult to be present when you’re with the baby
- Excessive hand washing or sanitizing
- Staying awake for fear that something will happen to the baby
- Avoiding activities like bathing the baby or leaving the house with the baby
Postpartum OCD Symptoms
Postpartum OCD occurs when OCD symptoms either develop or worsen shortly after giving birth. People who have just given birth are at increased risk of developing this condition during the postpartum period. These symptoms are often, but not always, associated with the new baby. For most people, symptoms begin within four weeks of delivery.3
Postpartum OCD Obsessions
Postpartum OCD obsessions generally center around harm coming to the baby in some way, whether intentionally or unintentionally, caused by you or by others.7 Obsessions generally center around contamination, sexual thoughts, harm, perfectionism, losing control, or religious content.7
Common postpartum OCD obsessions include:
- Fear of the baby getting sick or dying
- Having unwanted intrusive sexual thoughts about your own baby or fears that someone else will sexually harm the baby
- Fears of being a “bad” parent
- Fears of harming the baby, whether on purpose or on accident
- Intrusive images or thoughts of harm coming to the baby if things are not set up “perfectly”
- Fears of OCD symptoms actually being “proof” of psychosis or another serious mental health condition
- Fears of baby going to hell or suffering existential punishment because the parent did not pick the “right” religion
Postpartum OCD Compulsions
Postpartum OCD compulsions are mental or behavior acts believed by the person with OCD to lessen the chances of their obsessive thoughts coming true.7
Potential postpartum OCD compulsions could include:
- Not letting anyone else hold the baby, or going to excessive lengths to clean oneself before holding the baby
- Not letting anyone else change the baby, or asking someone else to monitor you while you change the baby
- Excessively cleaning the baby’s toys, foods, or belongings
- Comparing one’s parenting to other parents in an effort to “prove” to oneself that they are a “good” parent
- Only eating or drinking the “right” foods or drinks believed to be “safe” for the baby
- Going to excessive lengths to organize, arrange, or “perfect” baby’s environment
- Redoing caregiving behaviors if believed they are not done the “correct” way, or monitoring the other parent to make sure their caregiving is “correct”
- Excessive doctor visits or seeking reassurance from support system around caregiving acts
In order to be diagnosed with OCD, a person’s symptoms must negatively affect several different areas of their life, like school, work, and their relationships.
Why Do Obsessions & Compulsions Focus on the Baby?
Postpartum OCD can onset anytime between birth and eight weeks postpartum.9 The rapid shift in hormones from pregnancy to delivery, sleep deprivation, and the pressures of caring for a newborn baby all contribute to the increased risk of mental health concerns like OCD in the postpartum period. The content of the obsessions and compulsions experienced in postpartum OCD often reflect the intensity of parenting in the newborn days, with an intent focus on the well-being of the baby.
Will Obsessions About Violence or Sex Lead Me to Harm My Baby?
Experts agree that people dealing with postpartum OCD are not at risk of harming their babies.10 Obsessive thoughts, especially those about violence, sex, or harm coming to your baby, can be very distressing, but these thoughts will not cause you to harm your baby. In fact, the fact that you find the thoughts upsetting is a sign that you are dealing with postpartum OCD. You are not “going crazy” or a terrible parent. Getting properly diagnosed and treated can help you manage these thoughts and recover from postpartum OCD.
Treatment For OCD NOCD: Online OCD Treatment Covered By Insurance – Regain your life from OCD. Do live video sessions with a licensed therapist specialized in treating OCD. Treatment from NOCD is covered by most major insurance plans. Learn how you can use your insurance benefits. Visit NOCD Talkiatry: Is OCD Medication Right For You? Speak with A Doctor – Talkiatry can match you with a psychiatrist who takes your insurance and is accepting new patients. They’re in-network with major insurers and offer medication management with supportive therapy. Free Assessment
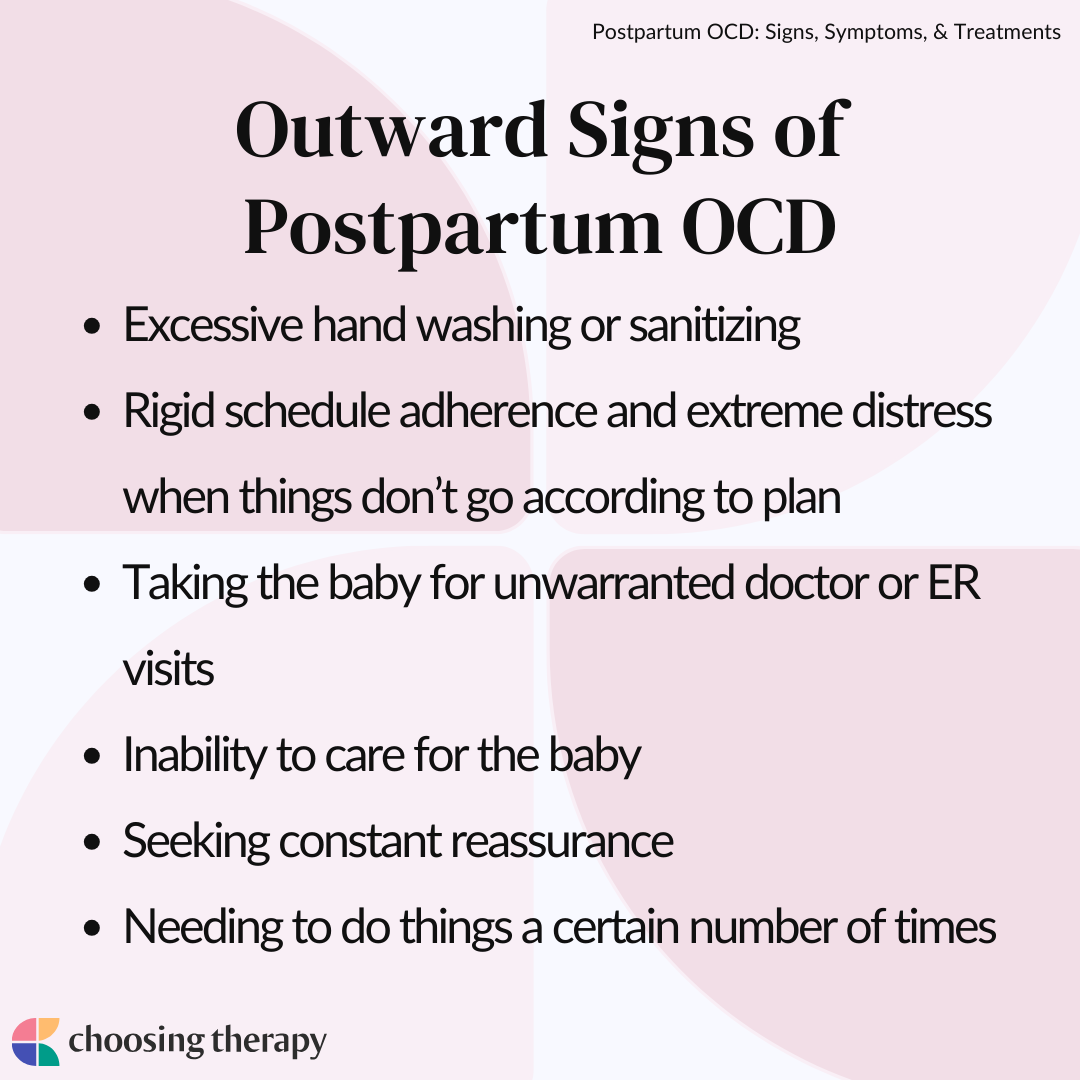
Outward Signs of Postpartum OCD
Although family members and friends cannot see the intrusive thoughts experienced by parents with postpartum OCD, there are things you can look for if you’re concerned that someone you love might be suffering from postpartum OCD.
Some outward signs that a new parent is experiencing postpartum OCD could include:
- Excessive hand washing or sanitizing
- Rigid schedule adherence and extreme distress when things don’t go according to plan
- Taking the baby for unwarranted doctor or ER visits
- Inability to care for the baby
- Seeking constant reassurance
- Needing to do things a certain number of times
Are Postpartum OCD and Postpartum Depression Related?
Some people confuse postpartum OCD for postpartum depression, but they are distinct disorders. Postpartum depression is a mood disorder, while postpartum OCD is an anxiety disorder that involves intrusive thoughts and compulsive behaviors that are difficult to control.
Postpartum OCD is one type of perinatal mood and anxiety disorder (PMAD), a class of mental health conditions that affect new and expecting parents. Postpartum depression is another type of PMAD that involves sadness, loss of interest in things, feelings of guilt and worthlessness, changes in sleep and appetite, difficulty concentrating, low energy, postpartum rage, and in severe cases, suicidal thoughts.11
Postpartum depression and comorbid OCD often occur together, meaning new parents suffer from both disorders at the same time.3 In fact, postpartum depression is the most common mental health disorder to occur alongside postpartum OCD. People with both disorders experience obsessions, compulsions, and depression that significantly interfere with their lives.
Postpartum Psychosis Vs. OCD
Postpartum psychosis is another type of mental health disorder that can develop after giving birth.3 It involves different types of disturbing thoughts, called delusions, also known as false beliefs or ideas that the person perceives as true. For example, a woman may believe that her baby is possessed by a demon.
Unlike people with postpartum OCD, those with postpartum psychosis are not distressed by their thoughts and beliefs, which increases their risk of acting on them. In some cases, this can lead to parents harming themselves or their babies. Someone experiencing postpartum psychosis requires immediate treatment and hospitalization. If you have concerns that someone you know is experiencing postpartum psychosis, seek help right away.
What Causes Postpartum OCD?
The exact causes of postpartum OCD are unknown, but researchers believe that it is likely caused by a combination of different factors, including hormonal shifts that occur post-delivery, the stress of caring for a newborn baby, genetics, and structural brain differences.
Common causes of postpartum OCD include:
- Hormones and OCD: Serotonin is a neurotransmitter that is responsible for regulating mood and emotions. Low levels of serotonin are linked to postpartum OCD. During the postpartum period, estrogen and progesterone levels decrease dramatically, which affects serotonin levels. These hormonal shifts are believed to play a role in the development of postpartum OCD.3
- Psychological stress: Caring for a newborn and adjusting to parenthood causes significant stress. New parents are also faced with sleep deprivation and little time to care for themselves. This increase in stress is another contributing factor to postpartum OCD.3
- Genetics: Family and twin studies show that there is a strong genetic link with OCD. Having a family member with OCD, especially a close relative like a parent or sibling, significantly increases the risk.12
- Differences in brain structure: Studies of people with OCD show differences in brain structure, including reduced gray matter in certain parts of the brain and lower amygdala volume.13
Risk Factors That Increase Likelihood of Postpartum OCD
Some experiences may increase the likelihood of someone developing postpartum OCD, including having a history of OCD during pregnancy or prior to pregnancy.3 Those with a history of depression, obsessive-compulsive personality disorder, and avoidant personality disorder are also at higher risk.13
Postpartum OCD is associated with a family history of mood disorders like depression and bipolar disorder, as well as substance use disorders. Other factors that may increase the risk of developing this condition include a history of miscarriage(s), first birth of a child, and experiencing complications during pregnancy or delivery.
What Are the Effects of Perinatal OCD?
Postpartum OCD can be very distressing for the new parent, and can affect how they bond with the new baby. People with this condition are also more likely to have marital problems and feel less confident in themselves. One study found that those with postpartum OCD responded less sensitively to their infants than parents without OCD.14
People with postpartum OCD are also more likely to experience postpartum depression (PPD). PPD can affect the parent/infant bond and is associated with cognitive and emotional problems as the child grows older.15 It is important to note that these studies looked at untreated postpartum conditions. If you’re experiencing postpartum OCD, getting treated can help you recover and reduce the likelihood of negative outcomes.
Can Postpartum OCD Be Prevented?
Attending all your postpartum appointments and sharing your concerns with your healthcare provider is important. Many providers schedule the first postpartum appointment six weeks after delivery, but symptoms of OCD or other PMADs can develop and worsen during this time. If you are experiencing distress, reach out sooner and request an earlier appointment.
Self-care is also an important component of preventing postpartum OCD. Be sure to take care of yourself by eating well, exercising (if approved by your healthcare provider), and getting enough rest. Sleep can be especially difficult while caring for a newborn baby, so consider asking your partner or a friend or family member to cover a night feeding so you can get a longer stretch of sleep, and try to sleep or rest during the day when possible. If you find that you are continuing to struggle with sleep, then you may be dealing with insomnia. Be sure to discuss this with your healthcare provider.
When to Get Help For Postpartum OCD
Seek help for postpartum OCD as soon as you recognize symptoms. Waiting can lead to the condition worsening, so it is important to reach out as soon as you notice intrusive thoughts. Untreated OCD can affect how you function in many different areas of your life, and it can also negatively impact your ability to care for yourself and bond with your baby.
How much do you know about OCD? Take This 11-Question OCD Quiz From NOCD. If you or a loved one are struggling with OCD, NOCD provides convenient, affordable, and effective OCD treatment covered by most major insurance plans.
How Is Postpartum OCD Diagnosed?
If you think that you are struggling with postpartum OCD, bring up your concerns with your OB/GYN, midwife, or other healthcare provider. They can assess your symptoms and provide you with a referral for treatment if needed. You can also seek help from a mental health professional, like a psychologist, therapist, psychiatrist, or psychiatric nurse practitioner. They will be able to evaluate your symptoms and discuss diagnosis and treatment options.
A simple way of finding a mental health professional in your area is by asking your primary care physician for a referral, or by using an online therapist directory. You can also utilize online OCD resources, like NOCD, which may be particularly convenient for new parents as treatment won’t involve leaving the house.
Postpartum OCD Treatment
There are several different types of treatment that can help you recover from postpartum OCD. Therapy and self-care are usually the first lines of treatment for this condition, especially for women who are breastfeeding. In some cases, medication and hormone therapy may also be helpful in combination with therapy and self-care strategies.
Exposure and Response Prevention
Therapy is an effective and widely used treatment for postpartum OCD exposure and response prevention (ERP) is a type of therapy recommended for this condition.3,16 ERP teaches people how to face anxiety-provoking thoughts, objects, and situations (such as the fear of dropping one’s baby) without resorting to rituals to alleviate the anxiety. Over time people learn to tolerate the anxiety caused by the intrusive thoughts and gradually stop their compulsive behaviors.
Couples Therapy
People with postpartum OCD may also benefit from couples therapy. Couples therapy can be helpful in educating people and their families about postpartum OCD.16 People with this condition may feel ashamed or guilty for feeling the way that they do, but by understanding their condition and sharing their experiences with a professional, they can learn to cope more effectively with their symptoms.
Medication
OCD medication is often recommended for moderate to severe postpartum OCD. Studies show that selective serotonin-reuptake inhibitors (SSRIs), like sertraline, fluoxetine, and paroxetine, are effective in treating this condition.3 They work by preventing the reuptake of serotonin, which increases the amount of it available in the brain. In some cases, other medications, like venlafaxine or quetiapine, may also be added to help enhance the effects of SSRIs.16
Some people with postpartum OCD have concerns about taking medication while breastfeeding. Research shows that most antidepressants are excreted in only small amounts in breast milk and do not have negative effects on the infant.16 If you are considering medication for your postpartum OCD, a psychiatrist or psychiatric nurse practitioner can discuss the pros, cons, and safety of it with you.
It is recommended that people with OCD continue taking medication for at least a year after remission to help prevent a relapse of symptoms.
Hormone Therapy
Hormone therapy may be used as a treatment for postpartum OCD.3 Research shows that there is a link between postpartum mood disorders and low estrogen levels. Some women with postpartum depression and psychosis have been successfully treated with the hormone estradiol and professionals believe that the same may be true for individuals with postpartum OCD.
Self Care
Self-care is another important component of recovering from postpartum OCD. Getting enough sleep, eating well, exercising, and connecting with a support network may not cure your OCD, but these actions, combined with treatment, can help you get better. It can be challenging to find time for yourself as you care for a newborn baby, but doing these things can help improve your emotional well-being and your ability to be a more present mother.
How to Cope With Postpartum OCD
If you are experiencing postpartum OCD, there are some actions that you can take to help support yourself in the road to recovery.
Here are several things you can do to help you cope with postpartum OCD:
- Remember that you are not alone. Nearly half of postpartum women deal with intrusive thoughts.
- Share how you are feeling with someone that you trust, whether it is a friend, family member, or therapist.
- Find positive outlets for your stress and anxiety, like exercise and meditation.
- Eat a healthy diet consisting of proteins, complex carbohydrates, fruits, and vegetables. Minimize sugar, caffeine, and alcohol.
- Be patient. Recovery from mental health disorders like OCD takes time.
- Don’t judge yourself for what you are experiencing. You are not a bad mother or person for struggling with OCD.
- Don’t turn to drugs, alcohol, or other addictive behaviors to help cope with your feelings. These activities may reduce your symptoms in the short-term, but will cause more long-term problems.
- Don’t isolate yourself. If you are struggling with postpartum OCD, reach out for help and get the support that you need.
How to Support a Partner or Loved One
It can be difficult to see a loved one struggling with postpartum OCD. If someone you care about is showing signs of this condition, there are ways that you can help support them. The first step is sharing your concerns in a gentle, non-judgmental manner. You can do this by stating something like, “I’ve noticed you doing more repetitive things lately and you seem very stressed.” People with postpartum OCD are usually distressed by their symptoms, so if they feel supported they may open up about their experience.
Once you have an open dialogue with your loved one, you can introduce the idea of getting help. You might share that you’ve done some research on postpartum OCD and learned that it is a treatable condition. If they’re open to it, you can share some resources or offer to help them find a provider. You may even offer to help bring them to the appointment, sit with them while they make phone calls, or watch the baby. If your loved one is not ready to get help, do not force it. Trying to force someone into treatment doesn’t work. Instead, respect their position and let them know that you’re there to help if they change their mind in the future.
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below. OCD Therapy NOCD: Effective, Affordable, & Convenient OCD Therapy Do live, face-to-face video sessions with a therapist who specializes in treating OCD and get 24/7 support between sessions. NOCD is covered by many insurance plans and is available nationwide. Visit NOCD Treatment From An Online Psychiatrist Talkiatry OCD is treatable. Talkiatry specializes in OCD and provides personalized care with medication and additional support. Get started with a short assessment. OCD Newsletter A free newsletter from Choosing Therapy for those impacted by OCD. Get helpful tips and the latest information. Sign-UpAdditional Resources
In My Experience
What to know when finding a therapist for OCD With so much information out there regarding providers and treatment options for obsessive compulsive disorder, it can be hard to know exactly where to start—especially when you have to consider everything from the type of provider to the different treatment methods, as well as how you’ll fit it into your busy schedule. Can OCD make it hard to make decisions? From choosing what to wear in the morning to picking what to eat for dinner, decision-making is a part of everyone’s daily routine. But for millions of people with Obsessive-Compulsive Disorder (OCD), making any choice can feel like a daunting, sometimes impossible task.