Research indicates a strong relationship between bipolar disorder and addiction.1 Though this relationship is not entirely understood, it is widely recognized that a co-occurring condition of bipolar disorder and addiction serves to exacerbate symptomology in both directions.1 Given that bipolar disorder and addiction are pervasive conditions, the experience may prove increasingly debilitating without appropriate intervention.
I’ve summarized important points on this topic in the video below:
Online Psychiatry Covered By Insurance
Talkiatry can match you with a real psychiatrist who takes your insurance and is seeing new patients. They’re in-network with major insurers and offer medication management. Get started with a short online assessment
What Is Bipolar Disorder?
Bipolar disorder sometimes referred to as “manic depression,” is a progressive neuropsychiatric condition grounded in genetics.2 The condition is met with emotional lability, meaning that individuals experience fluctuations in low-lows (depression) and high-highs (mania or hypomania). Bipolar disorder typically worsens with age, especially if left untreated. The disorder can be treated and often does stabilize, but not without consistent engagement in a disciplined process of medication and psychotherapy. For those who refuse treatment or go undiagnosed, symptoms will likely increase in intensity over time.2
Without diligent assessment, bipolar disorder can be challenging to diagnose. If, during an evaluation, a client presents as depressed and does not demonstrate any signs of mania, a specialist may readily diagnose the condition within the realm of major depressive disorder. Accordingly, if someone believes they may have a diagnosable case of bipolar, it is imperative to inform one’s provider of everything considered part of the condition. To do this, it is crucial to be aware of the general symptoms of bipolar disorder.
Common symptoms of mania in bipolar disorder include:7
- Feeling very up, high, elated, or extremely irritable or touchy
- Feeling jumpy or wired, more active than usual
- Decreased need for sleep
- Talking fast about a lot of different things (“flight of ideas”)
- Racing thoughts
- Feeling able to do many things at once without getting tired
- Excessive appetite for food, drinking, sex, or other pleasurable activities
- Feeling unusually important, talented, or influential
Common symptoms of a depressive episode of bipolar disorder include:7
- Feeling very down or sad, or anxious
- Feeling slowed down or restless
- Trouble falling asleep, waking up too early, or sleeping too much
- Talking very slowly, feeling unable to find anything to say, or forgetting a lot
- Difficulty concentrating or making decisions
- Feeling unable to do even simple things
- Lack of interest in almost all activities
- Feeling hopeless or worthless or thinking about death or suicide
Connections Between Bipolar Disorder & Addiction
Unfortunately, those diagnosed with either bipolar I or bipolar II disorder have a 30-50% or higher chance of developing alcoholism and substance use disorders.8 In fact, individuals experiencing mania are 14 times more likely to have a substance use disorder involving drugs and six times more likely to struggle with alcohol use disorder.8 In the opposite direction, those with a substance use disorder are 3.7-13.4% more likely to experience mania or hypomania than the general population.8 Accordingly, bipolar disorder and addiction feed off one another in a brutal fashion.
Similar connections between the development of bipolar disorder and substance use disorder include:
Desire to Self Medicate
Due to the overarching stigma on mental health and addictive disorders, many who would benefit from medication go without because they feel that treatment would make them “less than” others, which could not be further from the truth.
Unfortunately, this mindset often leads those experiencing either disorder to self-medicate through alcohol and other abusive substances. The issue here is that bipolar leads to an imbalance of neurotransmitters. The addition of foreign substances into the body, particularly those of abuse, only serves to disrupt homeostasis (neurochemical balance) further. Though the initial effect may feel desirable to the individual, it will eventually develop an accelerated pathway to addiction, from which many struggle to escape.
Abnormal Brain Structures
The prefrontal cortex (PFC) is best recognized for facilitating our morals and judgment. It is used for processing right from wrong while making safe and socially acceptable decisions. For individuals diagnosed with bipolar disorder, there is a noticeable difference in both the prefrontal and anterior cingulate cortices.10 Therefore, their problem-solving and concentration are significantly compromised.10 Additionally, the natural process of neurotransmitter and hormonal release and reuptake is compromised. While either condition may prove problematic for self and others, the two, in combination, yield increasingly complex risks. A similar abnormality is seen in the PFC in those with addiction, impacting their self-control and internal reward systems.11
The brain abnormalities seen in substance and bipolar disorders can lead to decompensation of:
- Attention processes
- Impulse control
- Memory
- Cognitive flexibility
- Affect (mood)
- Hygiene
- Productivity
Whether in the presence of psychotropic medication or not, substance use of any kind does compromise stability. While it is recommended that substance use be avoided entirely, those who decide to use are strongly urged to proceed with caution.
Genetic Predisposition
When considering any mental health disorder, it is crucial to assess the impact of nature versus nurture. Insofar as the “nature” piece, there is a genetic component in bipolar disorder and addiction that increases the likelihood of developing either if a parent had it previously. This predisposition is evident as there is at least a 40% lifetime prevalence of developing a substance use disorder for those with bipolar I disorder.12 If one’s biological parents are co-morbidly diagnosed with both, the likelihood of this is even more significant, especially if the child has learned to model the behaviors of their birth parent.
Help For Bipolar Disorder
Online Psychiarty For Bipolar Disorder – Talkiatry can match you with a real psychiatrist who takes your insurance and is seeing new patients. They’re in-network with major insurers and offer medication management. Most psychiatry visits cost patients $30 or less* Free Assessment
Talk Therapy – Get help from a licensed therapist that has expertise with bipolar. BetterHelp offers online therapy starting at $65 per week. Visit BetterHelp
*Includes copayment, deductible, coinsurance, and $0 Visits. Excludes no shows.
Does Substance Use Make Bipolar Symptoms Worse?
Substance use absolutely makes bipolar symptoms worse. We must consider how either condition is invasive and, in combination, symptomatology is heightened. One condition reinforces the other in a vicious cycle, effectively acting upon one another.
Substance use can impact the severity of bipolar disorders including:
- Intensified manic and depressive symptoms
- Increased aggression and agitation
- Longer and less manageable episodes
- Increased risk-taking behaviors
- Struggles to maintain a daily routine/schedule
- Higher rate of suicide
- Diminished quality of life
Can Addiction Cause Bipolar Disease?
It is more likely that an individual with bipolar disorder will succumb to addiction rather than the other way around. However, compromised brain chemistry stemming from addiction may increase the likelihood of developing bipolar disorder, especially for those with a genetic predisposition.
Given that bipolar disorder does entail some psychotic features, any substances that promote psychosis are especially compromising. Although many cases of substance-induced mental health disorders may subside over time with abstinence, those on the more prolonged substance use may have an increased likelihood of developing full-blown, chronic drug-induced bipolar disorder.13
Fortunately, there are warning signs a person can look out for if they suspect a loved one with bipolar disorder is abusing alcohol or substances. Should these warning signs be present, having a supportive, direct conversation with a loved one is advisable. The sooner, the better, as additional time misusing substances complicates the issue further.
When dating an alcoholic person with bipolar disorder, it is important to remember that alcohol is highly accessible to the public but is just as compromising as any other substance of abuse. In any case, you should address the issue as soon as it is noticed. Every moment counts.
Warning signs of substance and alcohol addiction in a loved one with bipolar disorder can include:
- Increased aggression or violence
- Further decline in self-care
- Social withdrawal or defensiveness
- Struggling with with the completion of important daily tasks
- Increased impulsive and high-risk behavior (impulse control disorder)
- Excessive spending on substance use
- Failure to engage in a medical regimen or treatment
- Thoughts or attempts toward harm to others or self (suicidal ideation)
Treatment for Comorbid Bipolar Disorder & Substance Use Disorder
It is highly recommended that someone with comorbid bipolar disorder and a substance use disorder seek treatment. Both conditions, in and of themselves, are chronic if gone unchecked, meaning they become more severe over time. Treatment is the first step in overcoming the adverse side effects of each disorder.
Once one becomes self-aware of the issue, it is essential to find a therapist. A therapist may work to help stabilize maladaptive thoughts, feelings, and behaviors. Given that bipolar disorder entails a chemical imbalance in the brain, it is highly recommended that a person adheres to a medication regimen prescribed by a psychiatrist. From here, a counselor and psychiatrist may work together to ensure one is stable both in life and physiologically.
Therapy
Therapy will not only address issues beyond the diagnostic conditions themselves, but also anything else problematic that may continually reinforce them. Treatment is an ongoing lifelong process for both, as there is no cure for bipolar disorder or SUD besides symptom management. Over time, therapy may become less stringent when one achieves maintenance, but it will always remain a part of one’s life.
Therapeutic options for comorbid bipolar disorder and SUD include:
- Cognitive behavioral therapy (CBT): During a CBT session for bipolar disorder, a client and counselor work together to identify maladaptive core beliefs and values that compromise thoughts, emotions, and behaviors.
- Motivational interviewing: This approach considers where one is at in terms of intrinsic motivation to change. Individuals may arrive in precontemplation (unaware of the issue/unwilling to change) or contemplation (aware and considering change). From here, therapy is devised to help the client move forward.
- Eye movement desensitization and reprocessing (EMDR): EMDR is an approach in which the therapist and client work to disconnect triggering stimuli from traumatic reactions. EMDR generally lasts 6-12 sessions, as needed.
- Solution-focused therapy: This is more of a short-term approach that seeks to find the source of the problem and remediate it quickly. Given the pervasive and chronic nature of bipolar and substance use disorders, this approach is often integrated into other forms of therapy.
- Family therapy: Whenever a family member struggles with a mental health or substance use disorder, others are impacted. Family therapy serves to get everyone on the same page insofar as meeting individual needs within the family context, minimizing arguments, enhancing interpersonal communications, and more.
Medications
Effective treatment of bipolar disorder often requires psychiatric medications. The medications for a co-occurring disorder vary widely, and stabilization may take some time. Though it is recommended to treat both the bipolar and addiction conditions concurrently, stabilizing the bipolar disorder first may yield positive benefits. Doing this helps ground the individual, which minimizes the desire to use substances as a coping skill. Further, bipolar medications may come with the additional benefit of reducing substance cravings.
Stopping medication abruptly or using it “only when necessary” may impair brain chemistry and functioning, which increases undesirable symptoms. Accordingly, consistency is essential. Some individuals may believe that bipolar medication is addictive, as it is required for stability. Keep in mind that when mood-stabilizing drugs are taken correctly, individuals are stabilized and are less likely to struggle with the symptoms of either condition.
Medication options for treating comorbid bipolar disorder and addiction include:
- Gabapentin
- Quetiapine
- Divalproex sodium
- Lamotrigine
- Serotonergic antidepressants*
- Olanzapine
- Olanzapine-fluoxetine* combination
- Lithium
- Risperidone
- Aripiprazole
- Pregabalin
- Benzodiazepines**
*These medications carry a black box warning, the most severe kind of warning from the FDA for the risk of suicidal thoughts and behaviors in certain people. You should talk with your doctor about these risks before starting this medication.
**This medication has black box warnings, the most severe kind of warnings from the FDA for abuse or misuse, risk of physical dependence, and risk of severe side effects, including death, when combined with an opioid.
Integrated Addiction Services
Beyond traditional forms of treatment, 12-step programs and others aim to address all aspects of life that might add to complications in managing someone’s disorders. Whether alone or in combination with treatment, they provide an opportunity for those struggling or in recovery to interact with others who share similar experiences. Doing this is cathartic as individuals recognize they are not alone. Here, one may receive support, become exposed to other resources, share stories, and be held accountable by peers.
Addiction treatment services that use and integrate approaches to mental health include:
- Rehab (inpatient and outpatient): These programs can last anywhere from 30, 60, to 90 days or longer. These typically involve individual therapy, group therapy, medication management, and other comprehensive approaches that enhance well-being and functioning.
- Intensive outpatient therapy/partial hospitalization programs: This treatment is less restrictive than rehab or inpatient programs but more restrictive than traditional outpatient. Individuals partake in extensive therapy throughout the week but have the option to work and reside at home.
- Medical detox: For more severe cases of substance use disorders, it may be necessary to begin treatment with a controlled medical detox. A medical professional facilitates this process, and withdrawal is carefully monitored and remedied through treatment measures.
Online Psychiatry Covered By Insurance
Talkiatry can match you with a real psychiatrist who takes your insurance and is seeing new patients. They’re in-network with major insurers and offer medication management. Get started with a short online assessment
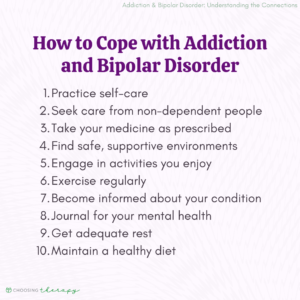
How to Cope With Addiction & Bipolar Disorder
Effective coping mechanisms can help reduce addictive behaviors in those with bipolar disorder and addiction. Substance use serves as a faulty remedy to bipolar and otherwise undesirable symptoms. By replacing maladaptive coping skills with healthy ones, individuals can better resume life in a healthy fashion.
Here are 10 strategies that can help you manage addiction with bipolar disorder:
- Practice self-care: Note that self-care is individualized and highly specific to the individual. Try engaging in healthy activities of personal interest that maximize well-being.
- Seek care from non-dependent people: Rather than rely on those who do not have your best interest in mind, rely on those who do—even if you may struggle with their helpful recommendations.
- Take your medicine as prescribed: This cannot be stressed enough! Bipolar disorder is not curable and requires ongoing therapy, which includes medication. When you feel better, it is a sign that the drug is working. Do not stop.
- Find safe environments: Some environments are more conducive to recovery than others. When the environment is unsupportive, remove yourself and relocate somewhere more supportive.
- Engage in activities you enjoy: Allow your passion for something healthy to engage you. This focus will remove you further from those who compromise your recovery.
- Exercise: Exercise releases healthy neurotransmitters such as endorphins, dopamine, and serotonin. These minimize pain while enhancing euphoric sensations naturally. An added benefit of exercise is becoming fit and improving physical appearance.
- Become informed: Healing begins with awareness. The more informed you are, the less likely one is to succumb to triggers.
- Journal: Journaling is cathartic. By expressing yourself on paper, you expel negativity and highlight positives. Additionally, having a record of progress and setbacks over time helps keep your recovery on track.
- Get adequate rest: When you sleep, cells rejuvenate, you become rested, thoughts are more clearly articulated, and homeostasis may be attained. Further, good rest reduces incidents of mania.
- Maintain a healthy diet: Eating more nutritious foods makes you feel healthier. Adequate nutrients may help further stabilize one’s body chemistry.
How to Help Someone with Comorbid Addiction & Bipolar Disorder
Attempts to help or support a friend suffering from addiction and bipolar disorder are most fruitful when thought out accordingly. Remember, both conditions are highly intrusive and pervasive, so the earlier the intervention, the better. First, becoming as informed as possible about both situations is essential. From there, explore available treatment options in one’s local area that are accessible in terms of location, finances, and provider specialty.
When helping someone with addiction, do so in a supportive, informed manner. Avoid becoming defensive or going on the attack while listening and offering to provide the support desired. This action may require you to make personal life changes such as abstaining from substance use, seeking therapy, and actively participating in their treatment.
When helping a loved one experiencing addiction with bipolar disorder, it is important to remember things such as:
- Being considerate and compassionate
- Realizing that both conditions are outside of their control
- Realizing that the issue is not about you but something they are struggling with
- Getting them the help they need
- Not feeding the issue further by encouraging substance use or lack of treatment adherence.
- Set a positive example by caring for yourself and practicing what you preach.
Final Thoughts
A co-occurring diagnosis of addiction and bipolar disorder may be discouraging, but there is hope. Adherence to a treatment regimen is one way people can begin living a more well-balanced life. Fortunately, treatment options are readily available and come in numerous forms. Remember that you are not alone. If you believe that you are struggling with addiction and bipolar disorder, help is out there. Your life is always one worth saving.
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
Online Treatment for Opioids or Alcohol, Including Medication.
Workit Health – Modern, personalized recovery that combines medication, a supportive community, and helpful content. Covered by many insurance plans. Currently available in FL, TX, OH, MI, and NJ. Visit Workit Health
Alcohol Treatment – Cut Back or Quit Entirely
Ria Health – Quickly change your relationship to alcohol with our at-home program. On average, members reduce their BAC levels by 50% in 3 months in the program. Services are covered by many major health plans. Visit Ria Health
Drug Addiction Rehab Centers
Recovery.com – Find the best local detox or drug rehab center covered by your health insurance. Search by location, condition, insurance, and more. Read reviews. Start Your Search
Telehealth Treatment For Opioid Use Disorder
Bicycle Health – offers therapy, support, and medication for addiction treatment (MAT). MAT offers the lowest relapse rates for opioid use disorder, helping people to stop using opioids with minimal physical discomfort. Covered by most major insurance. Visit Bicycle Health
Drinking Moderation
Sunnyside – Want to drink less? Sunnyside helps you ease into mindful drinking at your own pace. Think lifestyle change, not a fad diet. Develop new daily routines, so you maintain your new habits for life. Take a 3 Minute Quiz
Online Bipolar Test A few questions from Talkiatry can help you understand your symptoms and give you a recommendation for what to do next. Best Online Psychiatry Services Online psychiatry, sometimes called telepsychiatry, platforms offer medication management by phone, video, or secure messaging for a variety of mental health conditions. In some cases, online psychiatry may be more affordable than seeing an in-person provider. Mental health treatment has expanded to include many online psychiatry and therapy services. With so many choices, it can feel overwhelming to find the one that is right for you.

Find a therapist for bipolar disorder
Get the help you need from a therapist near you
City or zip Search